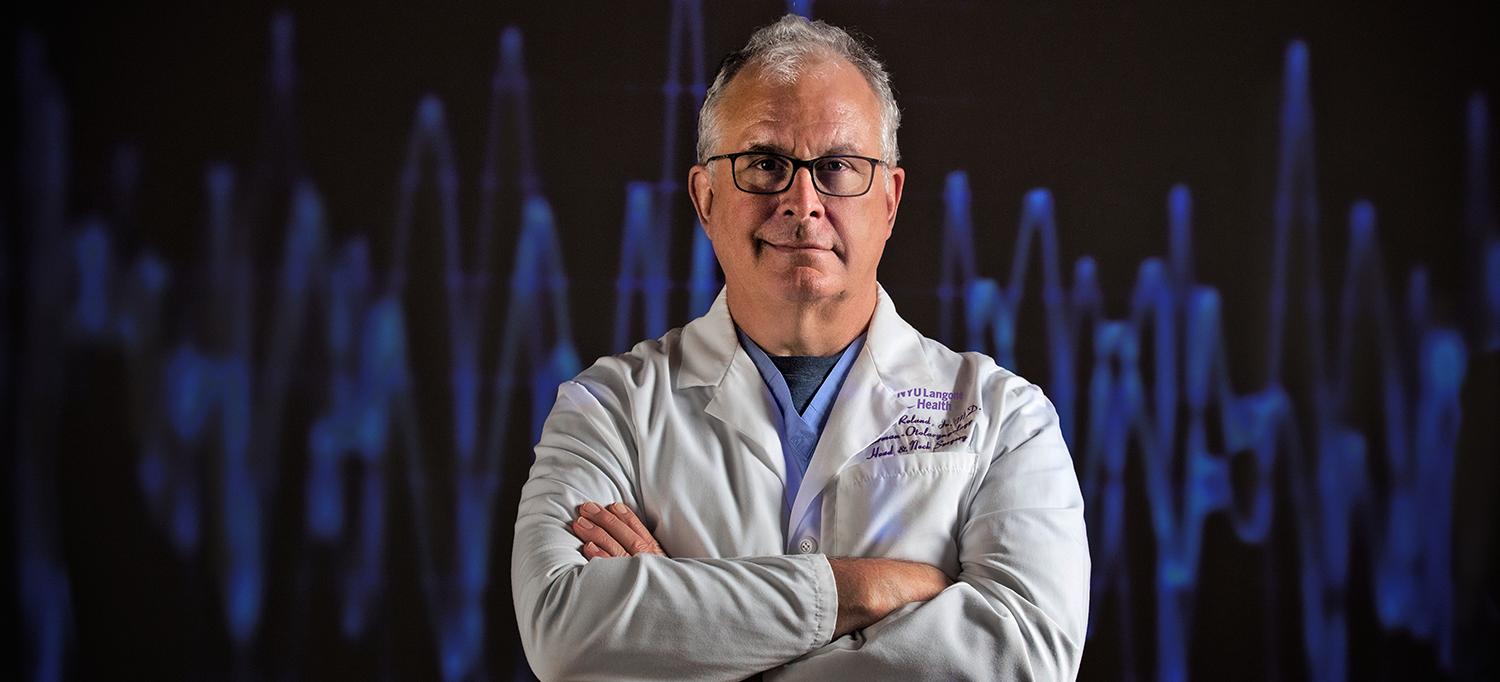
Building on a foundation of innovative research, Dr. J. Thomas Roland Jr. and the multidisciplinary team at the Cochlear Implant Center work to improve device performance and optimize patient outcomes.
Photo: NYU Langone Staff
As research sheds greater light on the optimal placement of cochlear implants (CIs)—and the brain’s adaptation to the device in order to process sound—experts at NYU Langone’s Cochlear Implant Center are working to fine-tune both the procedure and its postsurgical protocols. Discoveries from center experts are poised to enhance patient outcomes while also benefiting the quality, safety, and efficacy of the device itself.
Fine-Tuning Placement to Target Pitch
The effectiveness of CIs relies on the placement and circuitry of the device. To enhance sound quality, the placement approach should optimize the cochlea’s tonotopic anatomy—in which low frequencies are delivered to the top of the structure.
Prior research led by center investigators explored how CI electrode placement may correlate with enhanced sound processing without trauma to the inner ear. In one cadaver-based study, the novel implantation of a frequently used CI type was found to effectively stimulate the top of the cochlea while avoiding inner-ear damage by utilizing the device’s ground wire.
Based on findings in the earlier research, a second, human study led by J. Thomas Roland Jr., MD, the Mendik Foundation Professor of Otolaryngology and chair of the Department of Otolaryngology—Head and Neck Surgery, and David M. Landsberger, PhD, assistant professor otolaryngology—head and neck surgery, will now explore whether pushing current into that low-frequency region at the cochlea’s apex translates into lower-pitch precepts.
To evaluate performance, they will use a tool that measures the patient’s spectral resolution—the ability of the brain to process nuances in tone once information is received from the cochlea. If proven effective, the approach could pave the way to new electrode stimulation pathways that deliver better spectral resolution.
“This research opens up a whole new concept in terms of reaching the cochlea, which currently relies on using thinner, longer electrodes,” notes Dr. Roland. “By exploring the possibility that it’s more about the stimulation paradigm than the number of electrodes we use, we hope to find a pathway toward restoring more natural hearing.”
A Marked Focus on Surgical Quality
To ensure that cochlear implantation is as safe and efficient as possible, Dr. Roland and his team examine a number of quality improvement metrics for each surgeon, including surgical time, procedure cost, equipment usage, and complication rate. “The idea is to improve individual surgical performance, so that as a center we’re delivering an optimal operative experience for patients,” says Dr. Roland.
The collective emphasis on safety and efficiency has resulted in measurable metrics improvements, including a near-zero complication rate and a 20-minute reduction in average procedure time across more than 200 implantations in 2019. A credit to the center’s reputation for excellence, its specialists are consulted by a high volume of patients from across the country and the globe who seek correction or fine-tuning after their CI placement at other institutions.
This emphasis on quality and efficiency has led to the adoption of intraoperative monitoring, wherein an audiologist performs remote CI testing at the time of surgery. This makes the cost of a dedicated audiologist in the operating room unnecessary. It allows surgeons to confirm both the functionality of and patient response to the CI during the procedure itself via remote monitoring–facilitated, real-time communication with the operating room (OR).
An X-ray is also taken in the OR immediately following implantation, allowing the team to confirm that the electrode is in exactly the correct position. “If we didn’t, we could have to repeat surgery for a patient whose electrodes are rolled over or kinked—so before we leave the OR, we are certain that the device is functioning properly,” adds Dr. Roland.
Enhancing Efficacy—and Outcomes
After implantation, the effectiveness of cochlear implants relies heavily on programming expertise as well as the brain’s adaptation to signals from the device. Several ongoing translational research studies aim to normalize hearing while expediting the brain’s learning process to do so.
“We want to get ‘under the hood’ and figure out exactly how the brain acquires the implant’s electrical hearing sense, and why some do it better than others,” says Robert C. Froemke, PhD, associate professor of otolaryngology—head and neck surgery and neuroscience and physiology. “We need to understand at the neuron level what happens as the brain adjusts to the device, and how we can perhaps intervene in the process to bring slower learners up to speed.”
Expediting learning and enhancing the device’s performance can have a critical impact on outcomes for patients, for whom it can take several months or over a year to adjust to unusual sound intelligibility and initially subpar sound quality. Center researchers believe the process can be accelerated, and speech perception improved more immediately, with the use of neuromodulation. “The longer the adaptation process, the longer patients are straining to hear voices that sound, literally, like Mickey Mouse,” adds Dr. Froemke. “We’re hoping to shorten the timespan between initial stimulation and more natural hearing.”
Harnessing the Brain’s Plasticity
The length of the adaptation process relies on brain plasticity, the subject of neuromodulation research by Mario A. Svirsky, PhD, the Noel L. Cohen Professor of Hearing Science in the Department of Otolaryngology—Head and Neck Surgery. In one study, Dr. Svirsky is examining adaptation in patients who receive one cochlear implant for single-sided deafness (SSD). Using a specialized device, SSD CI recipients can manually adjust the acoustic input to their normal ear until it sounds as similar as possible to the CI, with initially unintelligible sound generally improving over time.
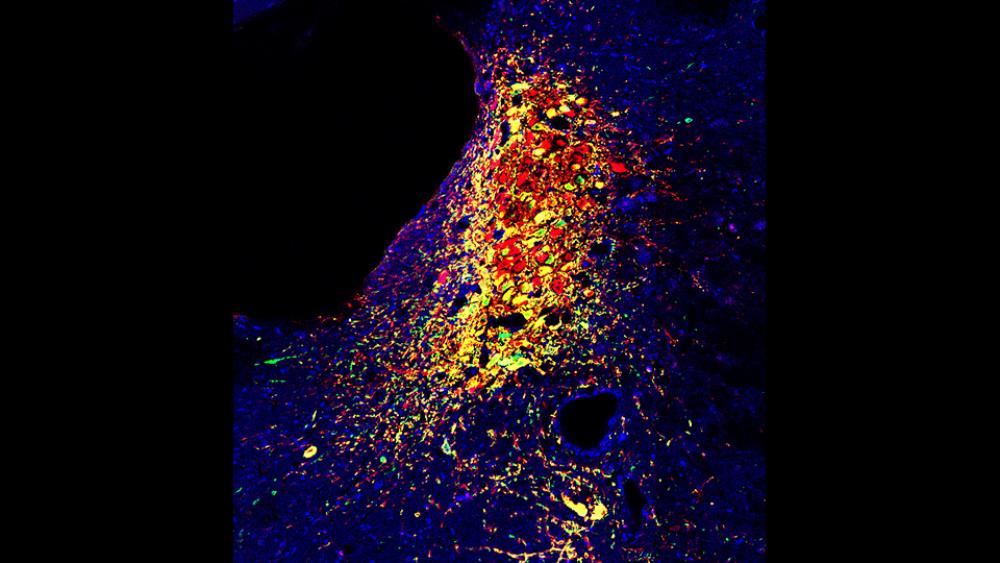
This insight has been applied to other, ongoing studies aimed at making the adaptation process faster or more complete. The Froemke and Svirsky laboratories are collaborating in an animal study where rats are trained to identify a specific tone following cochlear implantation. Researchers reward the tone by simultaneously using electrophysiology to stimulate a brain neurochemical center, the locus coeruleus, which is the first responder to sounds from the CI. The stimulation then releases noradrenaline throughout the central nervous system to alert attention, which appears to stimulate faster learning than in other animal subjects.
“Since we can’t ask animals what they hear, we have to train them to respond behaviorally and correlate the time it takes them to learn with different simulation patterns,” explains Dr. Froemke. “Some sounds might lead to reward, others may not—and we’re exploring how that dichotomy can inform electroacoustic integration.”
The study, presented at the Conference on Implantable Auditory Prostheses in July 2019, suggests that such a neuromodulation approach could be similarly used to expedite adaptation in human patients. “If we translate this to human patients and accelerate the normal adaptation process from a year to a month, that can make a tremendous difference to that patient’s quality of life—and acceptance of this intervention overall,” adds Dr. Froemke.
A Shared Emphasis on Discovery
These and other areas of research rely on meaningful multidisciplinary collaboration between clinicians and researchers in order to translate findings to the application of CI in practice, which leads to shared learning—at all levels. Dr. Roland has worked beyond his clinical practice to train student researchers to implant CIs in animal subjects, while Dr. Froemke and Dr. Svirsky have informed each other while undertaking parallel human and animal research projects. “Each side then informs what’s pursued and discovered on the other side,” notes Dr. Svirsky.
These discoveries ultimately inform quality care for more patients, in and beyond the center. As research helps patients with CIs experience better-quality hearing more quickly after implantation, experts believe the devices could better deliver on their potential to enhance patients’ quality of life. “If patients can experience better music appreciation, or function better at work or school—without the challenges of long training periods or compromises in hearing quality, we are hopeful it could encourage more patients to seek the benefits of cochlear implantation,” concludes Dr. Roland.