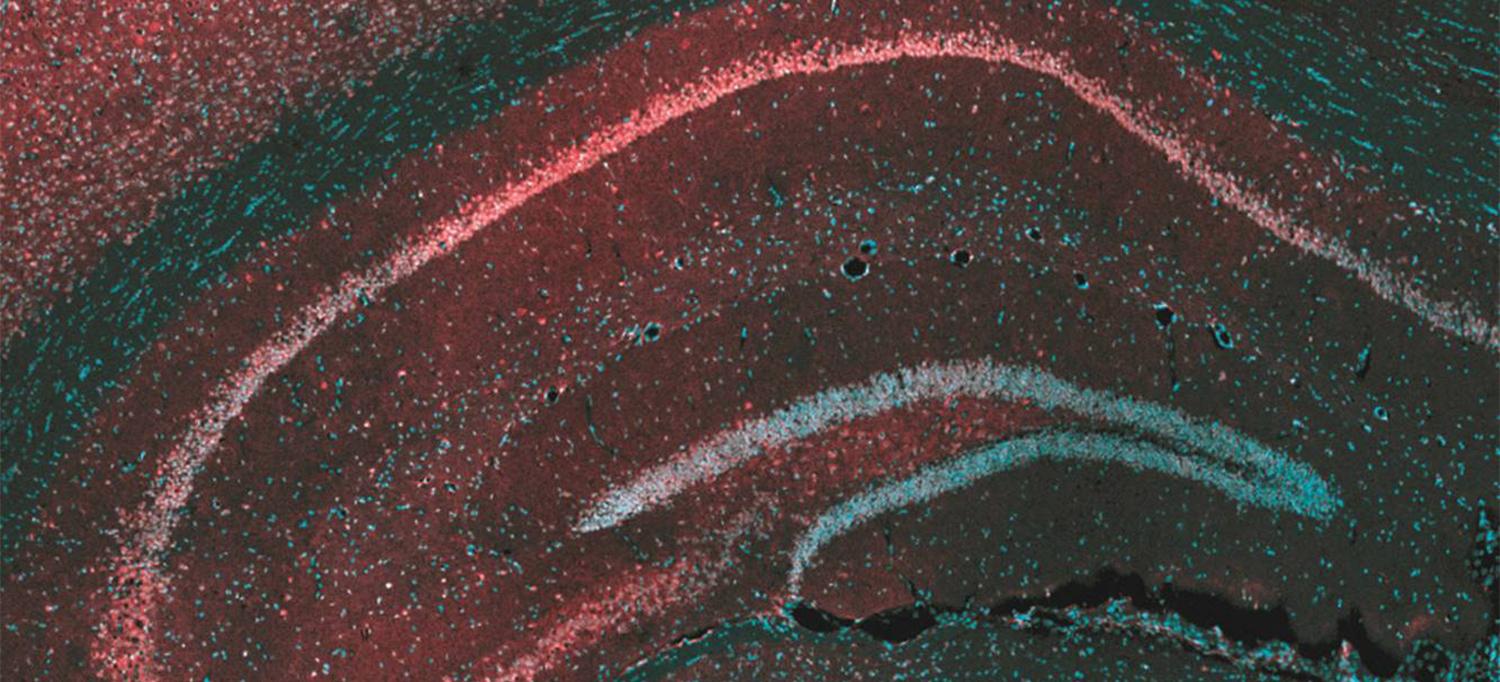
This microscope image of the brain region called the hippocampus shows the protein targeted by cannabis-derived CBD, GPR55 (red), and brain cells (blue) that send their extensions out to form the layers seen in the image. The interconnected nature of the hippocampus makes it a major site of for the initiation and spread of seizures.
Tsien et al. Courtesy of Cell Press
A study reveals a previously unknown way in which cannabidiol (CBD), a substance found in cannabis, reduces seizures in many treatment-resistant forms of pediatric epilepsy.
Led by researchers at NYU Grossman School of Medicine, the new study found that CBD blocked signals carried by a molecule called lysophosphatidylinositol (LPI). Found in brain cells called neurons, LPI is thought to amplify nerve signals as part of normal function, but can be hijacked by disease to promote seizures.
Published online February 13 in Neuron, the work confirmed a previous finding that CBD blocks the ability of LPI to amplify nerve signals in a brain region called the hippocampus. The current findings argue for the first time that LPI also weakens signals that counter seizures, further explaining the value of CBD treatment.
“Our results deepen the field’s understanding of a central seizure-inducing mechanism, with many implications for the pursuit of new treatment approaches,” says corresponding author Richard W. Tsien, PhD, chair of the Department of Physiology and Neuroscience at NYU Langone Health.
“The study also clarified, not just how CBD counters seizures, but more broadly how circuits are balanced in the brain,” adds Dr. Tsien, also director of NYU Langone’s Neuroscience Institute. “Related imbalances are present in autism and schizophrenia, so the paper may have a broader impact.”
A Disease-Causing Loop
The study results build on how each neuron “fires” to send an electrical pulse down an extension of itself until it reaches a synapse, the gap that connects it to the next cell in a neuronal pathway. When it reaches the cell’s end before the synapse, the pulse triggers the release of compounds called neurotransmitters that float across the gap to affect the next cell in line. Upon crossing, such signals either encourage the cell to fire (excitation), or apply the brakes on firing (inhibition). Balance between the two is essential to brain function; too much excitation promotes seizures.
The new study looked at several rodent models to explore mechanisms behind seizures, often by measuring information-carrying electrical current flows with fine-tipped electrodes. Other experiments looked at the effect of LPI by genetically removing its main signaling partner, or by measuring the release of LPI following seizures.
The tests confirmed past findings that LPI influences nerve signals by binding to a protein called G-coupled receptor 55 (GPR55) on neuron cell surfaces. This LPI–GPR55 presynaptic interaction was found to cause the release of calcium ions within the cell, which encouraged cells to release glutamate, the main excitatory neurotransmitter.
Further, when LPI activated GPR55 on the other side of the synapse, it weakened inhibition, by decreasing the supply and proper arrangement of proteins necessary for inhibition. Collectively, this creates a “dangerous” two-pronged mechanism to increase excitability, say the authors.
The research team found that either genetically engineering mice to lack GPR55, or treating mice with plant-derived CBD before seizure-inducing stimuli, blocked LPI-mediated effects on both excitatory and inhibitory synaptic transmission. While prior studies had implicated GPR55 as a seizure-reducing target of CBD, the current work provided a more detailed, proposed mechanism of action.
The authors propose that CBD blocks a “positive feedback loop” in which seizures increase LPI–GPR55 signaling, which likely encourages more seizures, which in turn increases levels of both LPI and GPR55. The proposed vicious cycle provides one process that could explain repeated epileptic seizures, although future studies are needed to confirm this.
Further, the current study examined the plant-based cannabinoid CBD, but the authors note that LPI is part of signaling network that includes “endocannabinoids” like 2-Arachidonoylglycerol (2-AG) that occur naturally in human tissues. LPI and 2-AG target receptors also regulated by CBD, but have different actions at the synapse. While LPI amplifies incoming electrical signals, endocannabinoids like 2-AG respond to increases in brain activity by dialing down the release of neurotransmitters from nerve cells. Interestingly, LPI and 2-AG can be converted into each other through actions of enzymes.
“Theoretically, the brain could control activity by toggling between pro-excitatory LPI and the restorative actions of 2-AG,” says first study author Evan Rosenberg, PhD, a postdoctoral scholar in the Tsien lab. “Drug designers could inhibit the enzymes that underpin LPI production or promote its conversion to 2-AG, as an additional approach to control seizures. LPI could also serve as a biomarker of seizures or predictor of clinical responsiveness to CBD, providing an area of future research.”
Along with Dr. Tsien and Dr. Rosenberg, study authors in the Department of Neuroscience and Physiology and Neuroscience Institute at NYU Langone were Simon Chamberland, Erica Nebet, Xiaohan Wang, Sam McKenzie, Alejandro Salah, Nicolas Chenouard, Simon Sun, and György Buzsáki, MD, PhD. NYU Langone authors also were Orrin Devinsky, MD, in the Department of Neurology, Rebecca Rose in the Division of Advanced Research Technologies, and Drew R. Jones, PhD, in the Department of Biochemistry and Molecular Pharmacology.
Additional study authors were Michael Bazelot, Shanice Bailey, Pabitra Hriday Patra, and Benjamin Whalley at the School of Chemistry, Food, and Nutritional Sciences, and Pharmacy at the University of Reading in the United Kingdom; Swati Jain and Helen E. Scharfman in the Departments of Child and Adolescent Psychiatry, Neuroscience and Physiology, and Psychiatry at NYU Langone and the Center for Dementia Research at the Nathan Kline Institute for Psychiatric Research; and Stuart Greenhill, Max Wilson, Nicole Marley, and Gavin Woodhall of the Aston Neuroscience Institute, School of Life and Health Sciences at Aston University in Birmingham, United Kingdom.
This work was supported by funding from the Ruth L. Kirschstein National Research Service Awards for Individual Predoctoral MD/PhDs (F30 NS100293) and a NYU Langone Medical Scientist Training Program Training Grant (T32GM007308), as well as by National Institutes of Health (NIMH) grant 5R37MH071739, National Institute on Drug Abuse grant DA040484-01, the Simons Foundation, the Vulnerable Brain Project, Finding a Cure for Epilepsy and Seizures (FACES), the Charles H. Revson Senior Fellowship in Biomedical Science, the Andrew Ellis and Emily Segal Investigator Grant from the Brain and Behavior Research Foundation, a postdoctoral fellowship from the Fonds de Recherche du Québec-Santé (FRQS), and a K99/R00 Pathway to Independence Award from NIMH (1K99MH126157-01). The services of NYU Langone’s Metabolomics Laboratory and Experimental Pathology Research Laboratory were supported by Perlmutter Cancer Center Support Grant P30CA016087.
Media Inquiries
Greg Williams
Phone: 212-404-3500
gregory.williams@nyulangone.org

