New research shows that women who receive mammography screening may have increased awareness of other preventive screening measures, which could affect patient counseling practices as well as health policies.
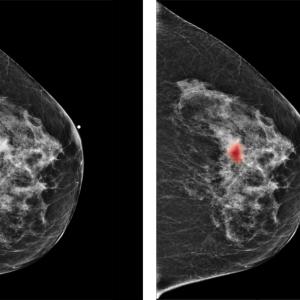
Photo: NYU Langone Staff
Medicare patients who undergo mammography screening also are more likely to follow up with other recommended preventive services such as cervical cancer screenings or Pap smear, bone mass measurement, or a flu vaccine, as compared to unscreened women, according to a new study led by researchers at NYU School of Medicine.
This study published online June 5 in Radiology, a journal of the Radiological Society of North America.
The researchers conclude that these findings, thought to be the first of their kind, could affect both policy and clinical practice.
“Screening has the potential to identify early disease that can be curable,” says senior study author and investigator Stella K. Kang, MD, assistant professor in the Departments of Radiology and Population Health at NYU School of Medicine. “It’s encouraging to see that women undergoing mammography may have increased awareness to other preventive screening measures.”
Dr. Kang points out that the main goals of the study were derived from the lack of research on the relationship between mammography and other preventive tests, or how false-positive results can impact a patient’s experience and utilization of other screening services.
The study consisted of 555,705 women age 65 and older. The 185,625 patients in the treatment group received mammography, while the 370,080 patients in the control group did not. Data also was collected on whether or not patients received additional preventive screening—including cervical cancer screening, also known as a Pap smear, bone mass measurement, or flu vaccine—within two years after a mammogram.
Based on standards from the American College of Radiology, results were categorized as true positive, requiring additional examination or imaging and a subsequent diagnosis of breast cancer within one year; false positive, a true positive result without a breast cancer diagnosis within one year; or true negative, showing no findings or benign findings.
Results of the study show that women with false-positive screening presented no difference in their likelihood of receiving a Pap smear or flu vaccine when compared to negative screening results. Overall, women who underwent the initial mammography screening were more likely to undergo additional preventive screening.
“In clinical practice, it’s important to understand that false-positives are generally well-tolerated and that patient anxiety is often short lived,” says Linda Moy, MD, study co-author and professor in the Department of Radiology at NYU School of Medicine. “But it’s still critical to address these factors in a dialogue with patients about an individualized care plan.”
Dr. Kang says that more research is needed to understand not only the impact of patient counseling and the patient experience as Dr. Moy suggests, but also how it impacts policy and how breast cancer screening could be a critical piece in bundling recommended preventive tests to women.
In addition to Dr. Kang and Dr. Moy, co-authors include Samantha Heller, MD, PhD, of NYU School of Medicine; and Miao Jiang, PhD; Richard Duszak Jr., MD; and Danny Hughes, PhD.