Credit: Getty/Md Babul Hosen
A certain biological pathway, a set of linked reactions in the body, drives the inflammation seen in the skin disease psoriasis, a new study finds. The work could lead to improved therapies for all inflammatory skin diseases, including atopic and allergic dermatitis, and for a type of boil called hidradenitis suppurativa, say the study authors. Inflammation is the body’s natural response to irritation and infection, but when out of control, it can lead to the reddish, flaky, itchy lesions that come with these skin diseases.
Led by researchers at NYU Langone Health, the new study showed that the interleukin-17 (IL-17) pathway, whose activity is blocked by existing anti-inflammatory drugs, activates a protein called hypoxia inducible factor 1-alpha (HIF-1-alpha) in psoriasis. Researchers say that IL-17 has long been known to be active in inflammation, but the role of HIF-1-alpha has until now been unclear.
The research team also found that HIF-1-alpha let inflamed skin cells more actively break down sugar for energy, supporting their metabolism and leading to the production of a waste product called lactate. When consumed by inflammatory T cells, lactate triggered production of IL-17, fueling even more inflammation.
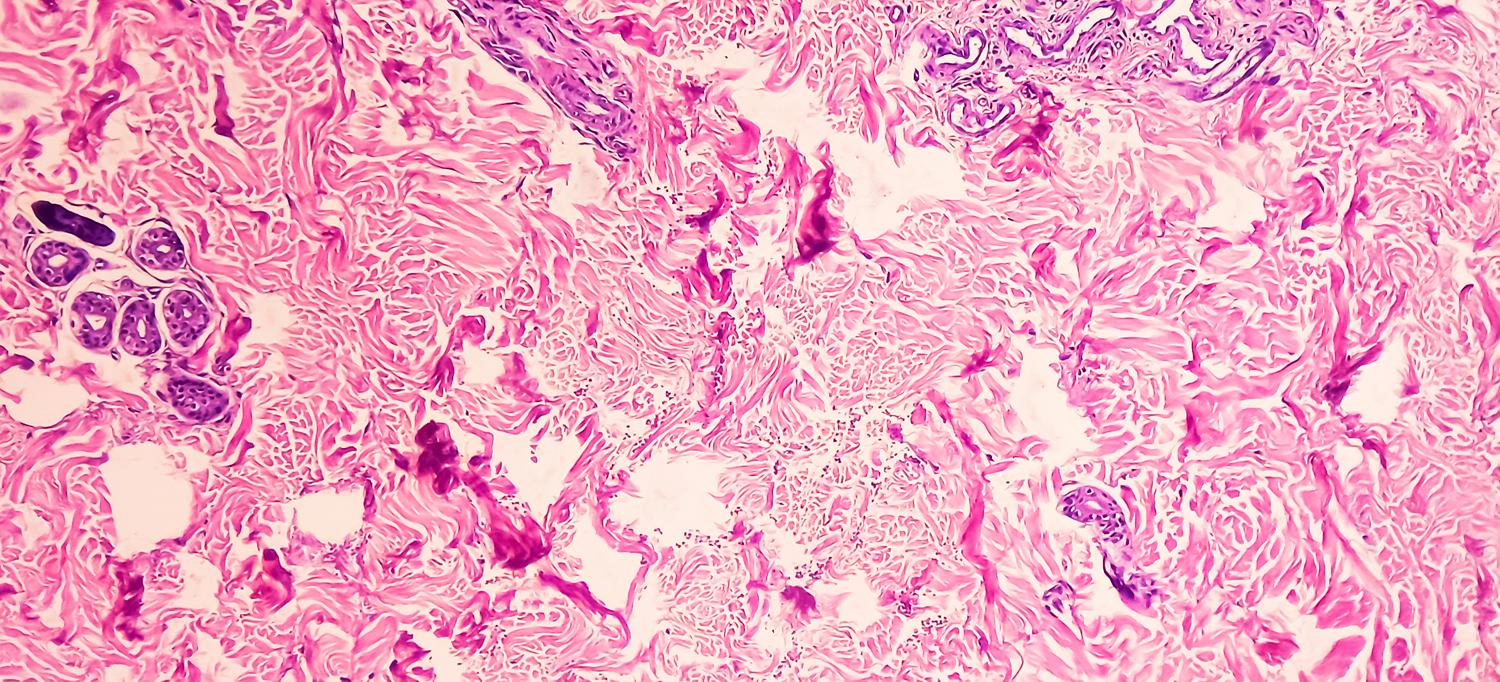
Published in the journal Immunity online May 20, the findings show that in human skin tissue samples from people with psoriasis, measures of gene activity around IL-17 and HIF-1-alpha were similar, suggesting that these factors are interconnected. Experiments in mice treated to develop psoriasis found that subsequent treatment with an experimental drug that blocks the action of HIF-1-alpha, called BAY-87-2243, resolved inflammatory skin lesions.
Further, skin samples from 10 patients successfully treated with anti-inflammatory drug etanercept showed diminished activity for both IL-17 and HIF-1-alpha, suggesting to researchers that when IL-17 is blocked, so is HIF-1-alpha.
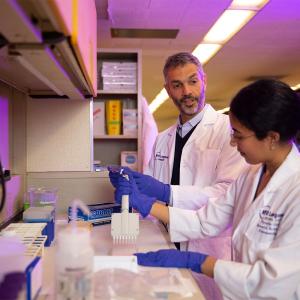
“Our study results broadly show that activation of HIF-1-alpha is at the crux of metabolic dysfunction observed in psoriasis and that its action is triggered by IL-17, another key inflammatory-signaling molecule,” said corresponding study author Shruti Naik, PhD, associate professor at NYU Grossman School of Medicine in the Departments of Pathology and Medicine, and the Ronald O. Perelman Department of Dermatology.
Further experiments were performed on skin samples from five patients with psoriasis whose healthy and inflamed skin was separately treated with either BAY-87-2243 or an existing combination topical drugs (calcipotriene and betamethasone dipropionate). Researchers then compared differences in inflammatory gene activity as a measure of impact, and found that the HIF-1-alpha inhibitor had a greater effect than existing topical drugs. Specifically, skin samples that responded to HIF-1-alpha therapy had 2,698 genes that were expressed differently, while standard-of-care–treated samples had 147 differently expressed genes.
Genetic analysis of skin samples from another 24 psoriatic patients treated with the IL-17–blocking drug secukinumab showed only decreased, not heightened, gene activity connected to HIF-1-alpha when compared to HIF-1-alpha gene activity in nine healthy patients with no psoriatic disease. Researchers say this indicates HIF-1-alpha’s blocked action was codependent on blockage of IL-17.
Additional experiments in mice showed that blocking sugar (glucose) uptake in the skin slowed psoriatic disease growth by limiting glucose metabolism, or glycolysis. Both the number of immune T cells tied to inflammation and the cell levels of IL-17 also decreased. The researchers found further that levels of lactate, the main byproduct of glycolysis, in psoriatic skin cell cultures dropped once exposed to the glycolysis-inhibiting drug 2-DG.
Directly targeting lactate production in psoriatic mice using a topical skin cream containing lactate dehydrogenase, which breaks down lactate, also slowed disease progression in the skin, with reduced numbers of inflammatory gamma-delta T cells and reduced IL-17 activity. Gamma-delta T cells were shown to take up lactate and use it to produce IL-17.
“Our findings suggest that blocking either HIF-1-alpha’s action or its glycolytic metabolic support mechanisms could be effective therapies for curbing the inflammation,” added Naik, who is also the associate director for NYU Langone’s Judith and Stewart Colton Center for Autoimmunity.
“Evidence of HIF-1-alpha’s depressed action, or downregulation, could also serve as a biomarker, or molecular sign, that other anti-inflammatory therapies are working,” said study co-senior investigator Jose U. Scher, MD, the Steere Abramson Associate Professor of Medicine in the Department of Medicine at NYU Grossman School of Medicine.
Scher, who also serves as director of NYU Langone’s Psoriatic Arthritis Center and the Judith and Stewart Colton Center for Autoimmunity, says the team plans to develop experimental drugs that can block HIF-1-alpha and lactate action in the skin “to end the underlying vicious cycle of IL-17–driven inflammation in skin disease. Our research fundamentally expands the scope of feasible therapeutic options.”
Naik points out that while many available therapies for psoriasis, including steroids and immunosuppressive drugs, reduce inflammation and symptoms, they do not cure the disease. She said further experiments are needed to refine which experimental drug works best, with respect to HIF-1-alpha inhibition, before clinical trials could start. Indeed, Naik and study co-lead investigators Ipsita Subudhi and Piotr Konieczny have a patent application pending for inflammatory skin disease therapies derived from their work on HIF-1-alpha inhibition.
More than 8 million Americans and 125 million worldwide are estimated to have psoriatic disease. The condition affects men and women equally.
Funding support for the studies was provided by National Institutes of Health grants P30AR075043, R01AR080436, R01AI168462, UC2AR081029, K22AI135099, K99AR083536, T32AR069515, TL1TR001447, UL1TR001445, and DP2AR079173. Additional funding was provided by the National Psoriasis Foundation, the Judith and Stewart Colton Center for Autoimmunity, the Beatrice Snyder Foundation, the Riley Family Foundation, the American Association of Immunologists, the International Human Frontier Science Program, the Charles H. Revson Foundation, and the Pew-Stewart Scholar Award 00034119, as well as the New York Stem Cell Foundation.
Naik serves on the advisory boards of Seed Inc. and as a consultant for BiomX. She also receives research funding from Takeda Pharmaceuticals. Scher has served as a consultant for Janssen, Pfizer, UCB, and BMS. He also receives research funding from Janssen and Pfizer. All of these arrangements are being managed in accordance with the policies and practices of NYU Langone Health.
Besides Naik, Scher, Subudhi, and Konieczny, other NYU Langone investigators were Aleksandr Prystupa, Rochelle Castillo, Erica Sze-Tu, Yue Xing, Daniel Rosenblum, Ilana Reznikov, Ikjot Sidhu, Cynthia Loomis, Catherine Lu, and Aristotelis Tsirigos. Other study co-investigators were Niroshana Anandasabapathy, at Weill Cornell Medicine; Mayte Suarez-Farinas, at the Icahn School of Medicine at Mount Sinai; and Johann Gudjonsson, at the University of Michigan.
Media Inquiries
Gregory Williams
Phone: 212-404-3500
Gregory.Williams@NYULangone.org