A protein–sugar molecule, CD99, occurs more frequently than normal on stem cells responsible for blood cancers, including acute myeloid leukemia (AML) and the related myelodysplastic syndromes (MDS). This is the finding of a study led by researchers from NYU Langone Medical Center and Memorial Sloan Kettering Cancer Center, and published online January 25 in Science Translational Medicine.
Building on this discovery, the study authors designed an antibody that recognizes and destroys CD99-covered leukemia cells while sparing normal blood stem cells, a finding confirmed by experiments in human cells and in mice with AML cells. Antibodies are immune system proteins that stick to a specific target, like a protein on the surface of invading bacterium. In recent years, researchers have become capable of engineering antibodies so that they target disease-related molecules.
“Our findings not only identify a new molecule expressed on stem cells that drive these human malignancies, but we show that antibodies against this target can directly kill human AML stem cells,” says corresponding study author Christopher Y. Park, MD, PhD, associate professor in the Department of Pathology at NYU Langone and its Perlmutter Cancer Center.
“While we still have important details to work out, CD99 is likely to be an exploitable therapeutic target for most AML and MDS patients, and we are working urgently to finalize a therapy for human testing,” says Park.
Direct Cell Killing
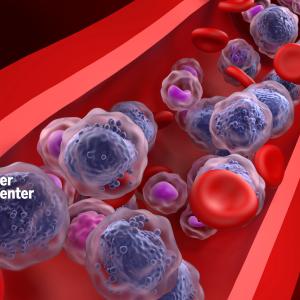
Acute myeloid leukemia and MDS arise from abnormal stem cells that build up in bone marrow until they interfere with normal blood cell production. People with these conditions may struggle with anemia, increased risk for infection, and bleeding.
The study results are based on the understanding that cancers, like normal tissues, contain stem cells that give rise to all the other cancer cells. Such “cancer stem cells” are known to be major drivers of many cancer types. In AML, a small group of leukemic stem cells become incapable of maturing into red or white blood cells as intended. Most leukemias respond initially to standard treatment, but relapse is common as standard treatments fail to kill leukemia stem cells, which continue to multiply.
The research team became interested in CD99 when they observed that it occurs frequently on AML and MDS cells, and then noted in the literature that CD99 is elevated in a rare bone cancer called Ewing’s Sarcoma. This prompted them to see if CD99 was important in the development of these blood diseases.
When researchers examined stem cell populations from 79 people with AML and 24 people with MDS, they found that approximately 85 percent of stem cells in both groups expressed high levels of CD99. The levels were so high that diseased stem cells could be cleanly separated from related, normal stem cells in people with AML.
Upon confirming that CD99 was abundant on leukemia stem cells, the research team then made several CD99 antibodies, and chose to focus on the one that most effectively killed those cells. Researchers found that when the study antibody attaches itself to CD99 on the surface of a cancer stem cell, it sends a signal inside the cell that increases the activity of enzymes called SRC-family kinases.
While the team does not yet know why, the binding of their antibody to CD99, and the subsequent activation of these enzymes, causes leukemia stem cells to die. Most cells with genetic mistakes leading to cancer sense they are flawed and self-destruct, but CD99, so the theory goes, may be part of a mechanism that prevents this. As the antibody binds to CD99, it appears to undo this block on self-destruction.
“With the appropriate support, we believe we can rapidly determine the best antibodies for use in patients, produce them at the quality needed to verify our results, and apply for permission to begin clinical trials,” says Park.
While AML is the most common acute leukemia affecting adults—with 22,000 new cases each year—it is expected to become more prevalent as the population ages, but AML is still relatively rare, accounting for 1.2 percent of cancer deaths in the United States. About 15,000 are diagnosed with MDS each year as well, mostly in older adults.
Along with Park, the study was led by Stephen Chung, William Eng, Wenhuo Hu, Mona Khalaj, Montreh Tavakkoli, and Ross Levine with the Human Oncology and Pathogenesis Program at Memorial Sloan Kettering Cancer Center. Also a study author was Virginia Klimek in the Leukemia Service at Memorial Sloan Kettering Cancer Center. In addition, Francine Garrett-Bakelman and Ari Melnick in the Division of Hematology and Medical Oncology at Weill Cornell School of Medicine, and Martin Carroll in the Division of Hematology and Oncology at the University of Pennsylvania, made important contributions.
Funding for the study was provided a Young Investigator Award from the Conquer Cancer Foundation of the American Society of Clinical Oncology, a U.S. Department of Defense Postdoctoral Fellow Award in Bone Marrow Failure Research (BM120096), a Fellow Scholar Award from the American Society of Hematology, a Clinical Scientist Award from the Doris Duke Charitable Foundation, a Translational Research Program Award from the Leukemia and Lymphoma Society, and a grant from the Geoffrey Beene Cancer Research Center.
Media Inquiries
Greg Williams
Phone: 212-404-3533
gregory.williams@nyumc.org