Study Led by NYU Langone Medical Center Looks at Calcium Channels as Regulators of Immune Responses to Tuberculosis
Many of us take a healthy immune system for granted. But for certain infants with rare, inherited mutations of certain genes, severe infection and death are stark consequences of their impaired immune responses.
Now, researchers at NYU Langone Medical Center have identified an important role for calcium signaling in immune responses to chronic infection resulting from Mycobacterium tuberculosis, the bacterium causing tuberculosis (TB).
Specifically, they determined that the immune systems in genetically altered mice lacking the critically important calcium channel component STIM1 failed to control TB, leading to severe lung inflammation and premature death. The researchers conducted their studies in mice because patients with mutations in the STIM1 gene and that of the channel it activates, ORAI1, are extremely rare and often too sick to study due to chronic infections and lymphoproliferative disease.
Results from the study are to be published online May 7 in the Journal of Clinical Investigation.
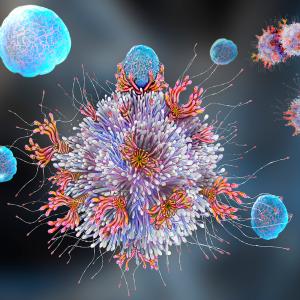
Under normal conditions, T-cells and other immune cells collaborate to mount an immune response to invading mycobacteria, ultimately controlling their growth. However, because Mycobacterium tuberculosis has developed many ways to evade the normal immune response, infections become chronic because a stalemate develops between the pathogen and the host.
“What we saw in mice lacking STIM1—whose T-cells cannot generate calcium signals—is that the number of mycobacteria in their lungs were dramatically increased, resulting in excessive inflammation,” says Stefan Feske, MD, associate professor of pathology at NYU Langone and the study’s senior author. “This was associated with an unexpected accumulation of T-cells in the lungs of infected mice that lack STIM1.”
Ludovic Desvignes, PhD, assistant professor of medicine at NYU Langone and one of the two first authors of the study, adds: “These T-cells produced large amounts of interferon-gamma (IFN-γ), an important protein mediator of immune response. This proved to be problematic because although IFN-γ protects against TB, too much of it results in harmful inflammation. We also found that the T-cells of STIM1-deficient mice could not be killed off, which normally is a mechanism that limits immune responses and avoids excessive inflammation.”
An additional mechanism to prevent the immune response from going “overboard,” the researchers conclude, is provided by a subset of T-cells called induced regulatory T-cells, or iTreg cells. These cells quench the function of T-cells and other immune cells, which participate in the immune response against the mycobacteria.
However, Dr. Feske and his colleagues found that calcium signals also are required for the development of iTreg cells, and that their numbers are strongly reduced in the lungs of the infected STIM1-deficient mice. They believe this further contributes to the severe lung inflammation in chronic TB.
“Our study highlights the important role of STIM1 and calcium channels in shutting down the immune response to chronic infection and in preventing injurious inflammation,” Dr. Feske says. “This shutdown mechanism surprised us because until now, we thought that calcium was needed to activate T-cells and immune responses to infection.”
VIDEO: Dr. Stefan Feske discusses the role of calcium signaling in immune responses to chronic infection.
Dr. Feske and his colleagues point out that their findings hold critical importance in further evaluation of the effects of new calcium channel inhibitors on immune responses to other chronic infections. His laboratory already has shown that by inhibiting calcium channels in T-cells, they were able to prevent T-cell activation in animal models of autoimmune diseases like multiple sclerosis and colitis. These preclinical studies suggest that inhibition of calcium channels may one day be used as a treatment for autoimmune diseases.
“Like in all immune modulatory therapies,” Dr. Feske adds, “the benefits of incomplete calcium channel inhibition need to be balanced against the dysregulation of the immune response that results when these channels are blocked completely.”
Several years ago, when Dr. Feske and his colleagues were at another institution, they were the first to identify ORAI1, a new calcium channel, which is essential for calcium influx and T-cell function. His laboratory also identified the first patients with inherited mutations in ORAI1 and STIM1 genes, showing that they lack calcium signals completely, causing defects in T-cell function and immunodeficiency.
Besides Drs. Feske and Desvignes, study co-investigators from NYU Langone include Martin Vaeth, PhD; Menghan Liu; Tawania Fergus; Lauren McVoy, MD, PhD; and Joel Ernst, MD.
The research was supported by grants from the National Institutes of Health (AI097302, AI065303, AI051242, and AI084041) as well as postdoctoral fellowships to P. Shaw from the National Multiple Sclerosis Society, and to C. Weidinger and M. Vaeth from the Deutsche Forschungsgemeinschaft (We5303/1-1 and VA882/1-1).
Disclaimer: Dr. Feske is co-founder of a small biotech company, CalciMedica, which develops CRAC channel inhibitors. The company was not in involved in the current study.
Media Inquiries
Jim Mandler
Phone: 212-404-3525
jim.mandler@nyumc.org