Doctors at the Brain and Spine Tumor Center, including Dr. Daniel A. Orringer, are using laser-based imaging and artificial intelligence to advance brain tumor treatment.
Photo: NYU Langone Staff
Recent advances at NYU Langone’s Brain and Spine Tumor Center—part of Perlmutter Cancer Center—are set to refine brain tumor treatment by targeting tumor tissue more precisely. With a novel intraoperative imaging system and collaborative drug trials, center experts are homing in on the nature and location of tumor cells in order to sharpen surgical and therapeutic treatment.
Real-Time Tumor Visualization Informs a Comprehensive Surgical Approach
A leading-edge imaging approach, developed by Daniel A. Orringer, MD, associate professor in the Department of Neurosurgery, provides unprecedented, near-real-time insight into tumor classification and visualization to ensure that no tumor tissue is left behind.
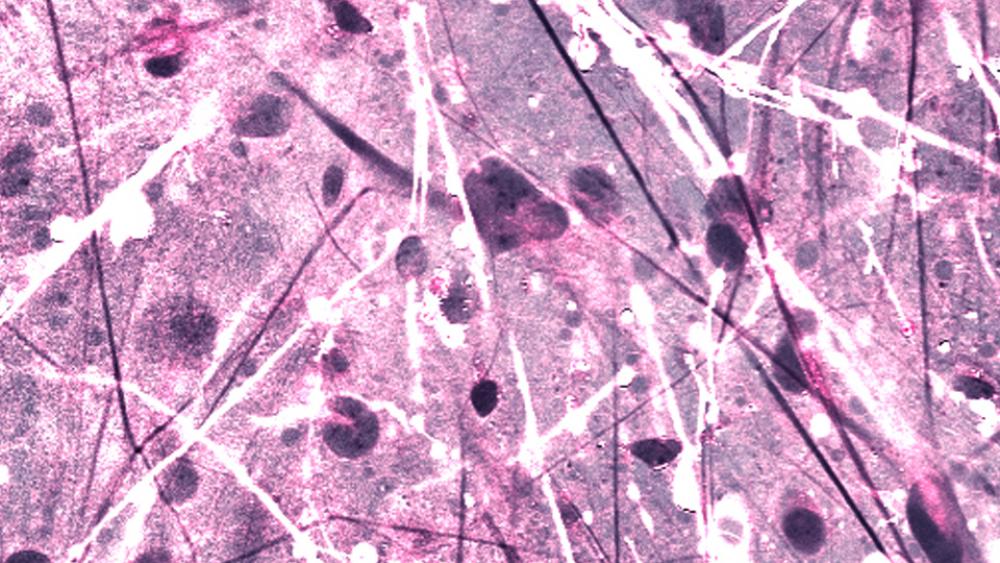
The laser-based imaging technique, stimulated Raman histology (SRH), is able to detect the degree of brain tumor infiltration in fresh, unprocessed human tissues by taking real-time microscopic images akin to traditional histologic slides. The imaging technique overcomes two long-standing challenges inherent to surgical brain tumor management: correct diagnosis of the tumor subtype at the time of surgery and accurate detection of residual tumor following resection.
“We know that patient survival and quality of life heavily rely on a safe and complete resection,” says Dr. Orringer. “Unfortunately, imperfect surgical outcomes are common, in part because of how difficult it is to visualize the margins of a tumor in the brain.”
SRH provides a new layer of intraoperative insight, shedding light on hidden tumor tissue that, despite traditional imaging and surgical prowess, can go undetected. Once the bulk of a tumor has been resected, SRH creates submicron-resolution images that reveal any remaining tumor tissue. Tissue samples are exposed to a laser beam, which detects and analyzes the light-scattering properties of biomolecules such as proteins, lipids, and nucleic acids. Tumor-infiltrated areas, abundant with protein and DNA, scatter light differently than normal, lipid-rich tissue, and the resulting contrast image provides more detailed information than histologic slides—without tissue processing, freezing, or staining.
Equipped with these virtual histologic images intraoperatively, surgeons can assess remaining tumor burden in surrounding tissues with unprecedented precision, completing surgical cases with previously unattainable levels of confidence in a tumor’s complete resection.
The newest addition to the center’s comprehensive suite of innovative neurosurgical imaging technologies, SRH works in concert with intraoperative MRI and fluorescence-guided surgery for high-resolution precision guidance. The technique can also help distinguish whether postresection MRI findings correspond to residual tumor or are simply the results of temporary inflammation due to resection.
“We’ve created a new paradigm for the way that we think about brain tumor surgery, one that integrates microscopic tissue architecture with our existing technology,” notes Dr. Orringer. “There is no other technology that allows for faster microscopic evaluation of tissue in the operating room.”
Imaging Combines with Artificial Intelligence for Automatic Diagnosis
In addition to conveying surgical treatment confidence with intraoperative insight, SRH also delivers a wealth of pathology information regarding a brain tumor’s subtype. Dr. Orringer and colleagues have paired SRH with state-of-the-art artificial intelligence (AI) algorithms to automatically categorize tumor tissue into 1 of 13 subtypes to inform their surgical management. In a prospective clinical trial of 278 patients at 3 institutions, the algorithm correctly classified 94 percent of tumors. Notably, the margin of error was in line with the findings of expert neuropathologists, with entirely nonoverlapping errors. “If pathologists were able to incorporate the insights from the algorithm, their accuracy would approach 100 percent,” Dr. Orringer says.
This precise diagnostic capacity is particularly beneficial for many centers nationwide that lack access to high-quality pathology labs and expert neuropathologists. “With our system,” says Dr. Orringer, “we can close that gap and essentially deliver out-of-box capacity to detect and diagnose brain tumors with accuracy traditionally found only in the most well-resourced centers.”
Even for well-resourced centers, the fast, accurate tumor diagnosis provided by SRH combined with AI can enhance rapid, real-time decision-making. “If we have a patient with tumor of unknown etiology, making the distinction in the operating room is extremely important,” notes Dr. Orringer. With the conventional workflow, surgeons often wait 30 to 40 minutes for pathology, whereas AI and SRH together can make that information available in less than 2 minutes. Rapid access to accurate pathology information will elucidate when tumor margins are best treated with further resection versus chemoradiation therapy—especially when tumor subtypes are known to respond to adjunct therapy—bringing surgical outcomes to new levels of quality and safety.
Developing Novel Therapeutics to Target Brain-Infiltrating Tumor Cells
As imaging and diagnostic breakthroughs improve surgical precision, investigators at the Brain and Spine Tumor Center are closing in on another line of attack on the brain-infiltrating tumor cells that may lay beyond surgical reach.
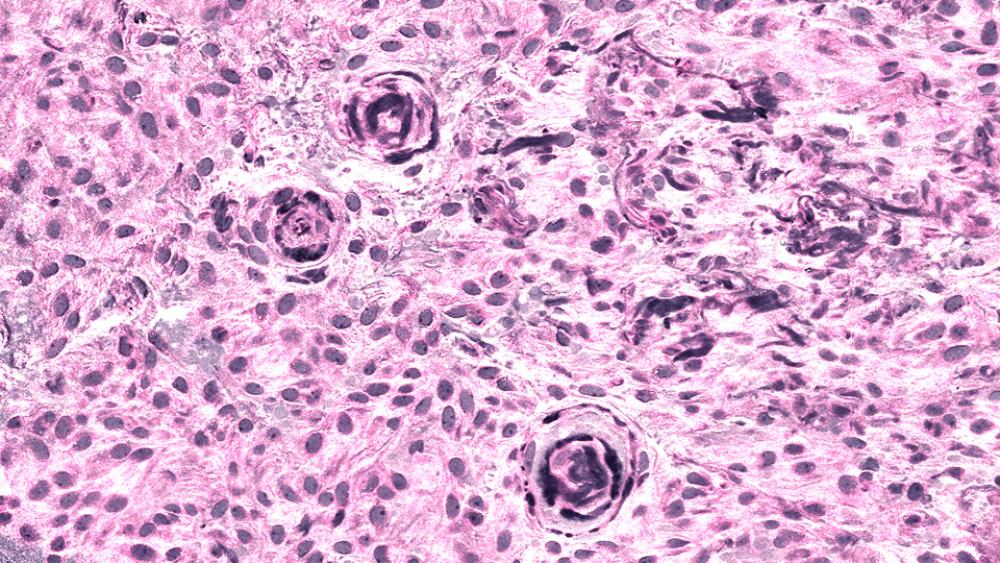
The newest advance builds on a previous discovery by a research team led by Dimitris G. Placantonakis, MD, PhD, associate professor of neurosurgery and director of the Neurosurgical Laboratory for Stem Cell Research. In 2017, the team identified a cell surface receptor, GPR133, expressed in glioblastoma cells but not in normal brain cells. “We know this receptor is necessary for glioblastomas to grow. When we take it away from the cells, they arrest and eventually die,” says Dr. Placantonakis.
In new work, the team described the expression profile of this receptor in glioma subtypes taken from a cohort of 67 archived glioma specimens at the center. The profile found that the receptor is de novo expressed in all gliomas, with the highest levels found in glioblastomas. While GPR133 was absent in the subventricular zone that harbors neural progenitors thought to give rise to gliomas, it was ubiquitously expressed in both the tumor bulk and in the brain-infiltrating tumor cells of gliomas, making it both a binary diagnostic tool and a promising therapeutic target.
As a G-protein–coupled receptor, GPR133 belongs to a receptor family whose members collectively make up the targets of one third of therapeutics on the market. But like many receptors in this family, GPR133 does not have any known ligand, as it is unclear what molecules it binds to.
“GPR133 has been classified as an orphan receptor because no one has looked for its ligand before,” Dr. Placantonakis says. “We are the first to do so, looking to understand which proteins or molecules may interact with this receptor.” The results of this search will help develop therapeutics that target only the glioma cells, with the goal of stopping their growth by shutting down the receptor.