With a central focus on quality and outcomes, Dr. Donato R. Pacione, and the entire surgical team in the Department of Neurosurgery, work to set the standard for patient care.
Photo: NYU Langone Staff
Enhanced by complementary expertise and leading-edge technology, a culture of quality and safety is driving decision-making across the Department of Neurosurgery. With forward-thinking treatment approaches and innovation-led advances in surgical precision, NYU Langone neurosurgeons are setting the standard for neurosurgical outcomes and enhancing patients’ quality of life—even as cases grow in both volume and complexity.
A Shared Definition of Quality Across the Care Spectrum
Propelled by a strong culture of quality and safety that permeates all levels of the institution, department-led initiatives build on a record of category-leading neurosurgical outcomes. At the same time, maintaining and enhancing the safety of patients’ postoperative care remains a critical emphasis as surgical volume continues to grow across locations.
“To set the standard for great neurosurgery, we take a deeper dive beneath the broader picture of medical quality and look carefully at quality care from both the surgeon’s and the patient’s viewpoint,” explains John G. Golfinos, MD, the Joseph P. Ransohoff Professor and Chair of the Department of Neurosurgery and professor in the Department of Otolaryngology—Head and Neck Surgery. “We want to create the best possible outcomes from our surgeries, then prevent the things that can happen during a patient’s hospital stay.”
Such a spectrum of continuous improvement includes adoption of the standard metrics of quality shared across NYU Langone, such as reduction of surgical site infections and venous thromboembolisms, as well as the enhancement of individual patient outcomes through neurosurgical advances, imaging innovation, and multidisciplinary partnerships. These goals are reinforced through quality and high-reliability organization rounds, along with regular quality improvement meetings to ensure that the emphasis on excellence is shared and reinforced.
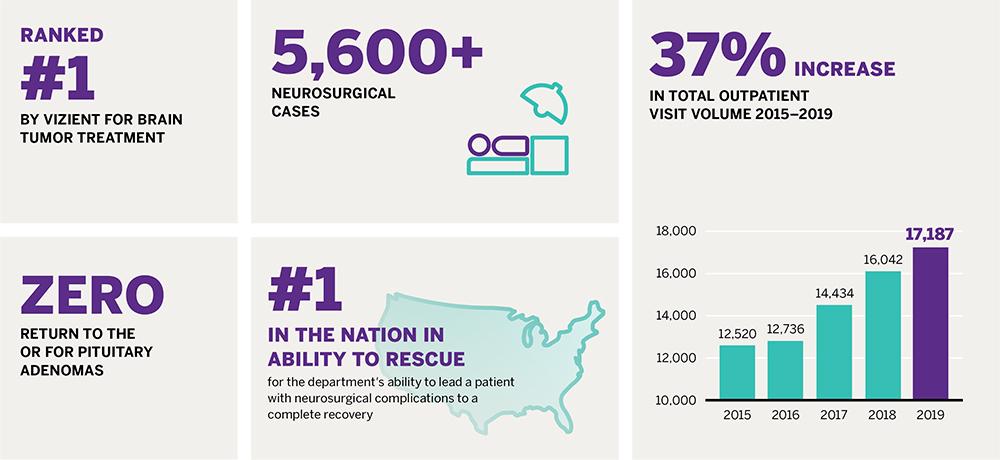
These and other enhancement measures are impacting overall quality metrics, supporting high performance in such categories as observed-to-expected mortality and failure to rescue, in which the department is ranked number one in the country for its ability to lead a patient who experiences complications to full recovery.
Advanced Tools Inform Surgical Approach
Investments in advanced intraoperative technologies, such as MRI scans, CT scans, and robotics, provide unprecedented visualization and precision, enabling highly skilled surgeons to more thoroughly resect tumors in less time. These technologies work together to clarify the margins of tumor versus normal tissue, elucidating the limits of the pathology in order to enable greater moderation in the surgical approach. “These tools are synergistic—they work better together to make tumor resection faster, smoother, and more accurate,” notes Dr. Golfinos.
For example, the pairing of intraoperative MRI with the department’s intraoperative frozen section microscope—one of just two nationwide—has substantially enhanced gross total resection rates while reducing repeat surgeries.
“You can take a specimen and, within five minutes, know whether you’ve reached gland tissue or there’s residual tumor,” notes Donato R. Pacione, MD, assistant professor in the Department of Neurosurgery. “With these tools together, you have greater confidence that you’re taking the bad and leaving behind the good.”
For benign pituitary adenomas, enhanced visualization of tumor margins, enabled by intraoperative imaging, has reduced the need for any additional surgery to address residual tumor to 0 over 12 months. For some pituitary tumors, advanced intraoperative imaging helps clarify the boundary between normal gland and tumor. This has not only improved rates of gross total resection but also reduced the rate of postoperative endocrinopathy. “This technology allows us to better balance aggressive resection with gland preservation,” notes Dr. Pacione. “And that impacts quality of life for our patients, who can avoid taking lifetime supplementation for a compromised pituitary.”
Rethinking Treatment to Reduce Harm
Following surgery, the emphasis on quality shifts to calibrating widely accepted treatment methodologies in order to prevent hospital-associated complications and enhance outcomes. With an evidence-based approach, the department is reexamining standard approaches to morbidities, such as infection, to identify whether they are effective in preventing harm—or costly, unnecessary interventions.
Dr. Golfinos and his team of neurosurgeons have reexamined the broad use of prophylactic antibiotics for the duration of the hospital stay in patients who undergo brain or spine surgery. “The axiom of treatment has been that if you cover everything with antibiotics, you’ll prevent infections,” notes Dr. Golfinos. “But who decided you have to put patients on antibiotics when they have drains put in? There was never any evidence behind that.”
To explore whether such antibiotic use reduces infection—or whether it puts patients at greater risk through drug resistance—the NYU Langone neurosurgical team began administering antibiotics only at the time of surgery, which is the minimal best practice recommendation from the American College of Surgeons. The new protocol was implemented using a stepwise approach starting with lower-risk patients and procedures: first, cranial surgery, then, minimally invasive spinal surgeries, all spinal surgeries, spinal drain catheters, and finally, endonasal surgeries, thought to be the highest risk in terms of bacterial exposure.
In studying more than 1,100 patients, 30-day infection monitoring revealed a reduction in post-operative infections along with a concurrent reduction in the drug-resistant organisms. Additionally, antibiotic-associated C. difficile colitis infections have been significantly reduced to just a single case in the last year, with a notable reduction in unnecessary care costs. Results of the initiative have been published in the Journal of Neurosurgery, Journal of Neurosurgery: Spine, and the British Journal of Neurosurgery. The department is working internally within the health system and externally with specialty societies to identify ways to disseminate its findings and transform standards of care in neurosurgery across other institutions.
“Not only are we using fewer antibiotics, but now we don’t have to worry about resistance as much, and when patients do get infections, now they’re less virulent,” adds Dr. Golfinos. “We can avoid unnecessary treatment and our patients do better—that’s good antibiotic stewardship.”
A Supportive Shift in Culture
These evolutions in care, notes Dr. Pacione, are a result of the structure of the department, where complications are met with immediate treatment or surgery, as well as an emphasis on patient quality at the cultural level. Such shifts, core to all neurosurgical practices within NYU Langone, requires forward thinking, top-down leadership—and constant reassessment.
“It’s in the fabric of our department to identify what great neurosurgery looks like and continue to work toward that,” says Dr. Pacione. “It means doing things others aren’t doing because there’s a return in that for our patients—and we’re beginning to see the metrics to support that these efforts are creating better outcomes.”