Photo: Juliana Thomas
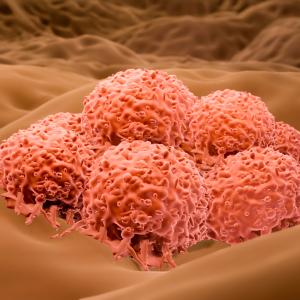
While it is well known that the majority of cancer deaths are caused by metastasis—and not by the primary tumor—the mechanisms behind metastasis are still not well understood. Now, a team of researchers at NYU Langone Health’s Perlmutter Cancer Center, led by Eva M. Hernando-Monge, PhD, professor in the Department of Pathology, and Iman Osman, MD, the Rudolf L. Baer Professor of Dermatology in the Ronald O. Perelman Department of Dermatology and professor in the Departments of Medicine and Urology at NYU Grossman School of Medicine, has been awarded a U54 grant (1U54CA263001-01A1) by the National Cancer Institute (NCI) to build an in-depth transcriptional and cellular map of tumor microenvironment interactions that regulate early dissemination of metastatic cells in melanoma.
“The National Cancer Institute recognizes that understanding metastasis is the next frontier in developing new therapies for cancer,” says Dr. Osman, also director of the Interdisciplinary Melanoma Cooperative Group at Perlmutter Cancer Center. “Melanoma is a perfect model to study early dissemination because disease recurrence happens even when tumors of a few millimeters in thickness are resected.”
With this award, the Perlmutter Cancer Center team joins four other multidisciplinary Metastasis Research Network (MetNet) teams in U54-supported Specialized Centers around the country as part of the NCI’s collaborative initiative.
Early dissemination of metastatic tumor cells is a relatively new concept in cancer biology, Dr. Hernando-Monge says. Previously, it was thought that primary cancer cells had to undergo a number of alterations before they gained the ability to leave their primary tumor site and disseminate to colonize distant tissues and organs. With the help of single-cell genomics and the ability to capture small amounts of tumor cells circulating in the blood, evidence now shows that tumors already contain cells that are able to disseminate and metastasize to other organs during the earliest stages of tumor development.
The Perlmutter Cancer Center MetNet includes three projects. Aims of the projects include mapping the cellular and molecular evolution of primary melanomas and their local and regional microenvironments to identify critical “switches” that drive nonlinear tumor progression; mechanistically dissecting the emergence and functional relevance of transcriptionally defined cell state heterogeneity of malignant and nonmalignant cell populations; and identifying novel therapeutic vulnerabilities to intercept early dissemination, mobilize systemic immune surveillance, and improve patient outcomes. The researchers expect that information gained through these projects should define new biomarkers of melanoma metastasis and therapeutic strategies to manage early disease.
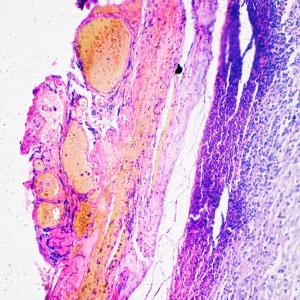
Research done through the MetNet initiative relies on novel mouse models as well as tissue samples from nearly 5,000 patients—one of the nation’s oldest and largest biobanks of melanoma specimens—collected by the Melanoma Research Program.
“In all of these, we will examine early-stage patient samples and identify candidates for functional studies which will be conducted in clinically relevant mouse models, and vice versa, findings in mouse models will inform the analyses of patient tissues,” Dr. Hernando-Monge says.
Other members of the Perlmutter Cancer Center MetNet are Mayumi Ito, PhD, professor in the Ronald O. Perelman Department of Dermatology and Department of Cell Biology; Markus Schober, PhD, associate professor in the Ronald O. Perelman Department of Dermatology and Department of Cell Biology; Amanda W. Lund, PhD, associate professor in the Ronald O. Perelman Department of Dermatology and Department of Pathology; Itai Yanai, PhD, professor in the Department of Biochemistry and Molecular Pharmacology; and Kelly V. Ruggles, PhD, associate professor in the Department of Medicine at NYU Grossman School of Medicine.
“Through the projects supported by the NCI-MetNet initiative, we can begin to develop a comprehensive picture of the earliest events leading to melanoma dissemination, and we may identify processes that drive metastatic dissemination in other cancer types as well,” Dr. Osman says.