Photo: Ed Reschke/Getty
Amanda W. Lund, PhD, a member of NYU Langone Health’s Perlmutter Cancer Center, joined NYU Langone in 2020 from Oregon Health Sciences University (OHSU), where she was an associate professor of cell, developmental, and cancer biology at OHSU School of Medicine.
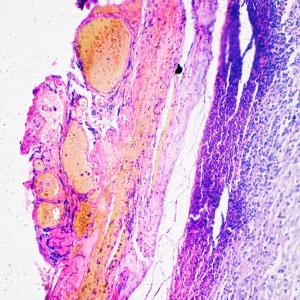
An associate professor in the Ronald O. Perelman Department of Dermatology and Department of Pathology at NYU Grossman School of Medicine, Dr. Lund studies the lymphatic vasculature, which plays an important role in clearing body tissues of the excess fluid and cells that build up within them. On the return trip into the blood, immune cells in the lymph nodes survey the contents to identify threats and activate an immune response, if needed.
Dr. Lund received the 2022 AACR-Bristol Myers Squibb Midcareer Female Investigator Grant at the recent American Association for Cancer Research annual meeting.
Here she discusses the relationship of the lymphatic vasculature to cancer, her research to better understand this system and its role in cancer metastasis, and more.
What is the lymphatic vasculature, and why is it important in cancer?
Lymphatic vessels are a crucial part of our circulation. Unlike blood vessels, which move nutrients and oxygen through all of our tissues, lymphatic vessels are a one-way route out of tissue, moving lymph through lymph nodes and ultimately back into the blood. The reason they are important is they play a critical role in maintaining fluid homeostasis (balance), are the critical routes for trafficking of immune cells, and play an important role in lipid transport. Their normal function is required for tissue homeostasis and health, and we think their dysfunction in the context of cancer has two main important impacts.
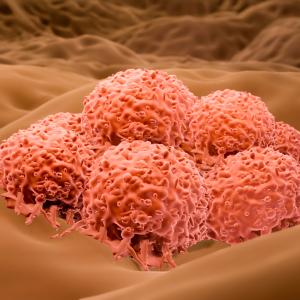
First, as they expand and respond to the developing malignancy, lymphatic vessels can provide routes for tumor cells to exit and metastasize to lymph nodes. We know that for many solid tumors, the presence of tumor cells in lymph nodes is an early event and poor prognostic for patients. As we have studied these vessels in the context of cancer, we have also learned that, as the critical route for leukocyte (white blood cell) migration out of tissues, they are required for immune surveillance against tumors. They allow the host to see a developing malignancy and initiate antitumor immune responses. But then, through mechanisms that we in the field don’t fully understand, they also can contribute to the tumor’s ability to evade the immune system.
Our lab is interested in understanding what the signals are that move through this system to regulate these different immunological processes and how the evolution of that immune response against the tumor can also contribute to metastasis and eventually poor outcomes for people with cancer.
What are some of the research projects that your lab is working on?
One of the projects that I am very excited about, which we have been working on for several years, is understanding the dynamics of T-cell movement out of tumors. The field of cancer immunology has appreciated that the CD8 T cell—the killer T cell—is a vital component of response to immunotherapy. These are the cells that are protecting patients on checkpoint inhibitor therapy. The more we understand how killer T cells work and how we get them into tumors, the better. Yet one aspect that has gone unappreciated is the dynamics of not only what gets T cells into the tumor microenvironment, where they can exert their killing function, but whether or not they stay in that environment, or if instead they recirculate out. When they recirculate out, they do that via the lymphatic vasculature.
We have been investigating those “stay and leave” signals and trying to understand what the mechanisms are that tell a T cell that found its target to stay versus maybe move on and continue to survey other tissues. We think that tumors put up a lot of barriers to T-cell retention, and the lymphatic endothelium in the tumor itself seems to be promoting the exit of a broad, diverse, functional set of T cells. We have been exploring these mechanisms in order to think about whether or not we could block the exit of T cells from the tumor in order to boost retention, and, ultimately, response to immunotherapy. That has led to a lot of additional questions—which we are exploring—regarding the role of lymphatic recirculation and how the lymphatic endothelium itself informs that process. That has been an exciting area for us.
Since moving to Perlmutter Cancer Center, my lab has also become much more engaged in understanding how lymphatic transport—the movement of cells, fluid, antigens, and soluble factors from the tumor to the lymph node—begins to co-opt and hijack lymph nodes very early during tumor progression in order to make them a hospitable site for a tumor cell. We know in mouse models that if we put tumor cells into a normal, healthy lymph node, they do not grow. So, there must be events that occur before the tumor cell’s arrival, driven by lymphatic transport, that prepare the lymph node for metastasis.
We have a really exciting project funded by The Mark Foundation for Cancer Research on this question in which we track proteins that are shed by the primary melanoma and transported via lymphatic vessels to the lymph node. We have identified exciting candidate molecules that are driving metastatic potential in the lymph node. This has led us to ask some additional questions, including to what extent the metastatic behavior is dependent on immune suppression and how this impacts systemic dissemination of tumor cells. There is a whole suite of changes that happens in lymph nodes in the mouse: How do these changes determine progression, and can we then translate those changes into the human setting to think about predicting which patients are at risk for progression?
Overall, the research that is going on in my lab is following an exciting trajectory.
Does your research focus solely on melanoma?
We have focused on melanoma, but in addition to the cancer work that we do, we also conduct a lot of basic immunology research in the skin. Comparing and contrasting what we find within the same tissue has been informative for us. We are, however, really excited by ongoing conversations with researchers who study other tumor types. We think that the kinds of questions we are asking are relevant across tissues. We are excited to continue to build these collaborations here at Perlmutter Cancer Center and think broadly about lymph node biology and lymphatic transport in cancer.
What does receiving the AACR-Bristol Myers Squibb Midcareer Female Investigator Grant mean to you, and what plans do you have for the funding it provides?
The award is an incredible and exciting recognition by my peers, for not only what we have done to push the question of lymphatic involvement and immunotherapy forward, but also for our potential over the next several years. It is really an honor to be recognized in that way. There are unique challenges for women in science at every career stage, so this mechanism, which recognizes someone who has advanced to the early mid-career stage, will provide the funds that allows my program to grow and ask cutting-edge questions.
What we have proposed to use the funding for is an extension of the first project that I discussed, which is this idea that T cells make a decision of whether to stay in the tissue or to leave. We think that there is a lot of really exciting work to be done in understanding the unique populations of T cells that are seeded in the tumor-draining lymph node. They are likely to be very responsive to immunotherapy and may directly control newly arriving metastatic tumor cells. How these T cells form, the nature of their relationship with the primary tumor and this egressing population that we’ve identified, and how they fail are important questions to study.
How will your research ultimately benefit people with cancer?
We are thinking of benefits in two ways. First, I think that the work we are doing to understand the interplay between the host immune response and the lymphatic vasculature might lead us to novel combination therapies, ways to target how the host “sees” the tumor in conjunction with immune checkpoint blockade, for example. Second, we are also thinking about the trafficking behavior of T cells as potential engineering strategies for chimeric antigen receptor (CAR) T-cell therapy. Again, this probably will not be specific to melanoma.
Fundamentally, lymphatic transport is engaged very early in tumor progression. And a lot of the biology that we are looking at is operating at the earliest stages in the patient. We have become more successful treating metastatic disease. I think we have the opportunity to think about these early mechanisms and how we might intercept disease progression to keep people with cancer from reaching an end-stage metastatic state. There are a lot of challenges to doing that; for example, identifying the patients that are actually at high risk for disease progression and determining whether the mechanism we are targeting is operative in that subset of patients. However, that is the direction we are heading: How do we identify patients early, and how do we direct care in those patients with high risk to interrupt disease progression?