Photo: STEVE GSCHMEISSNER/Getty
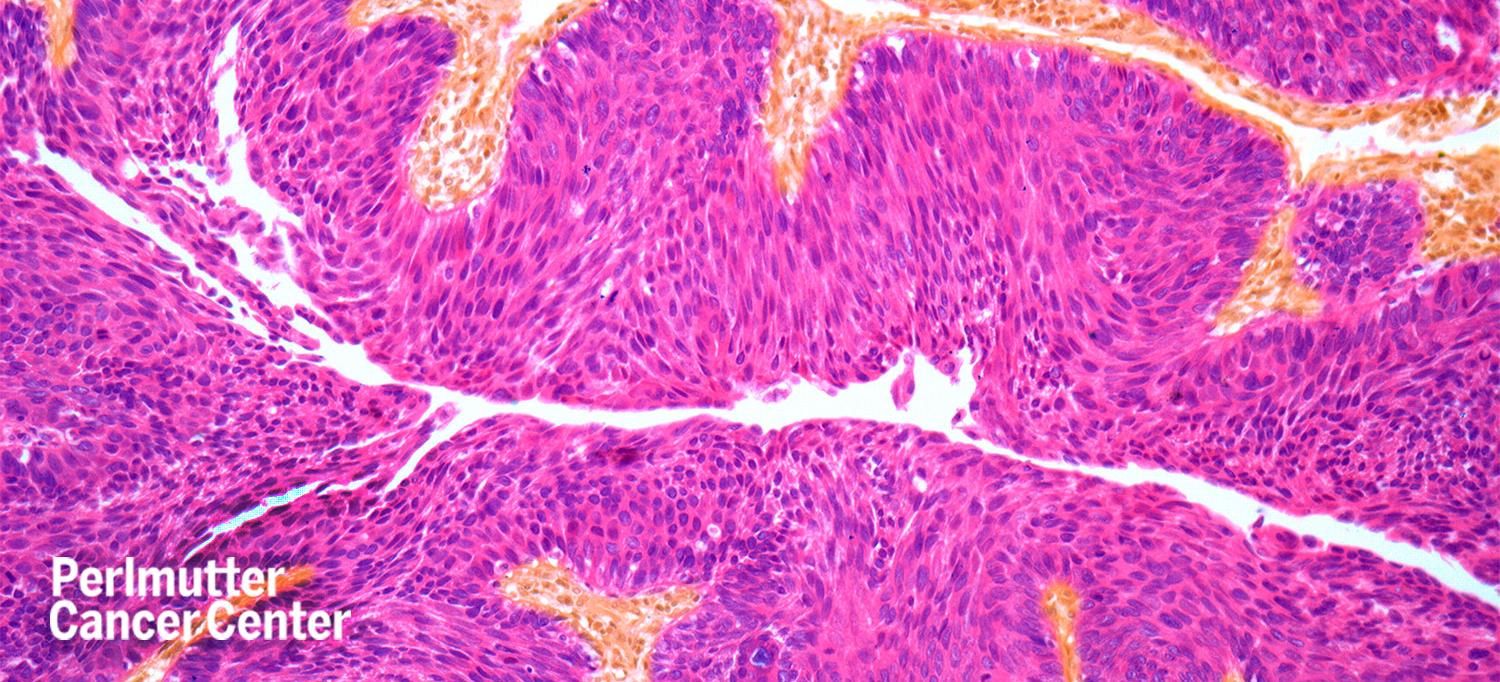
A newly opened clinical trial at NYU Langone Health’s Perlmutter Cancer Center aims to bring an innovative new treatment to people with a common form of bladder cancer.
Approximately 75 percent of all patients who have bladder cancer are initially diagnosed with a form of the disease called non-muscle invasive bladder cancer, with at least half presenting with high-grade, meaning more aggressive, cancer.
The current standard of care for people with high-grade non-muscle invasive bladder cancer is an intravesical medication called bacillus Calmette-Guérin (BCG). However, BCG does not work in over 30 to 40 percent of people with bladder cancer, driving the search for new drugs for initial, first-line, and second-line treatment of this disease, which may be associated with significant complications, alteration of quality of life, and mortality.
Gary D. Steinberg, MD, professor in the Department of Urology at NYU Grossman School of Medicine and director of the Goldstein Urology Bladder Cancer Program at Perlmutter Cancer Center, is conducting a phase 1 clinical trial to test a targeted cancer treatment. The novel type of therapy uses an antibody-drug conjugate for people with high-risk, non-muscle invasive bladder cancer that has recurred despite treatment with intravesical BCG. Perlmutter Cancer Center is the first of 12 sites in the United States to open for enrollment of participants.
The antibody-drug conjugate under investigation, enfortumab vedotin, carries a tumor-killing drug called monomethyl auristatin E (MMAE). MMAE is linked to an antibody that targets nectin-4, a receptor found on the surface of many cancer cells, but particularly in bladder cancer. Enfortumab vedotin delivers MMAE directly to the tumor, eliminating the cancer cells without harming healthy adjacent cells.
In December 2019, the U.S. Food and Drug Administration (FDA) granted accelerated approval to enfortumab vedotin for people with advanced bladder cancer that has progressed despite treatment with two previous therapies.
“Enfortumab vedotin is very effective, and it has revolutionized metastatic bladder cancer treatment,” says Dr. Steinberg, who helped develop the trial and is a member of the trial’s steering committee. “Our hope is that enfortumab vedotin can ultimately replace BCG as a first-line treatment for people with high-risk non-muscle invasive bladder cancer in its earliest stages.”
People with metastatic bladder cancer receive enfortumab vedotin intravenously, and like all intravenous chemotherapies, systemic side effects occur. Intravesical enfortumab vedotin may eliminate side effects such as peripheral neuropathy and rashes without sacrificing the drug’s effectiveness in the bladder, Dr. Steinberg says.
Currently, the standard of care for patients who have bladder cancer that does not respond to intravesical BCG is radical cystectomy, surgical removal of the bladder, with reconstruction of the urinary tract using the patient’s intestines. The FDA recently approved an immunotherapy medication called pembrolizumab as an alternate therapy for BCG-nonresponsive non-muscle invasive bladder cancer. Importantly, while there is a 40 percent complete response rate after three months of pembrolizumab treatment, only about 19 percent of the total participants that started the clinical trial that led to the FDA’s approval of the immunotherapy were still disease-free after 12 months.
“We are looking for a treatment that is more efficacious and has potentially fewer side effects than pembrolizumab so that patients can be cured of their cancer without surgical removal of their bladder,” Dr. Steinberg says. “We believe intravesical enfortumab vedotin will be a game changer for high-risk non-muscle invasive bladder cancer.”

