The Transplant Institute Has Performed More Than 100 Lung Transplants. This Was Its First for a Patient Whose Lungs Were Damaged by the Virus.
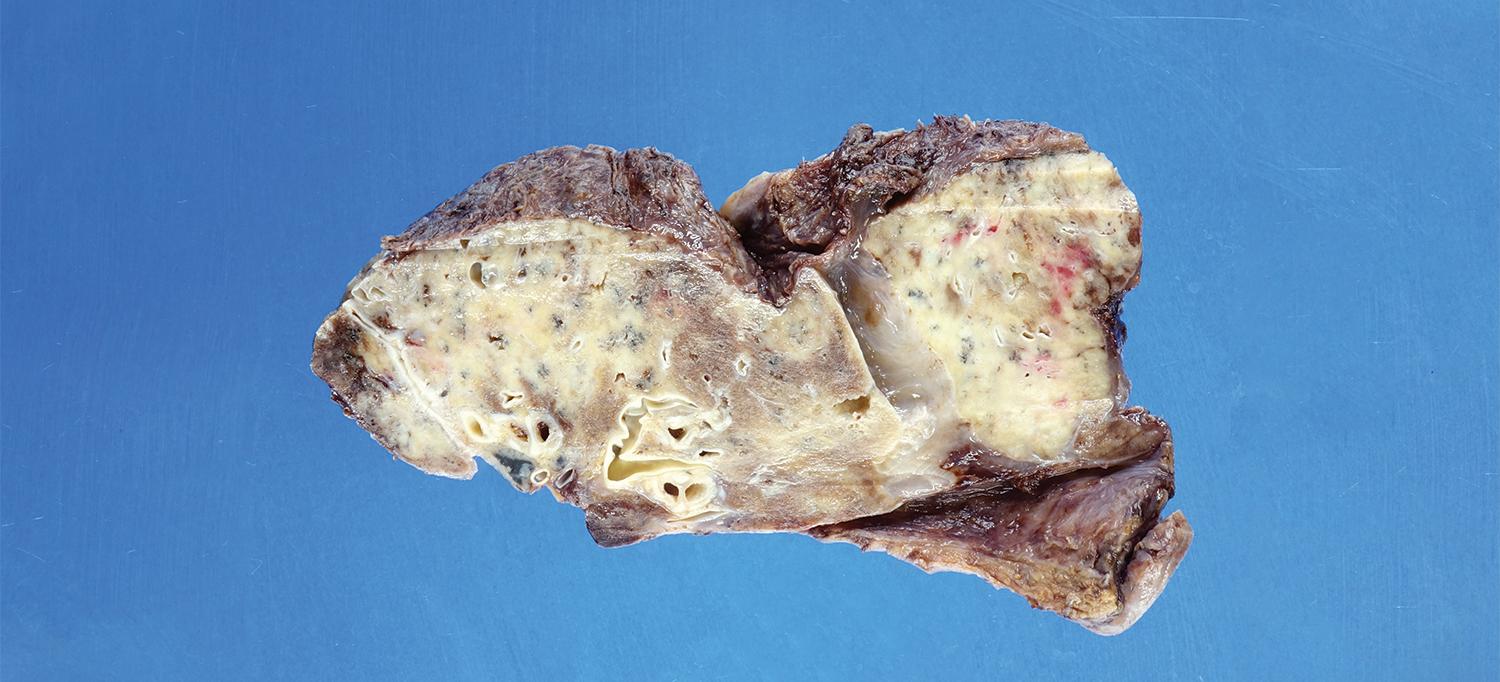
A virus-ravaged lung removed from a 47-year-old patient shows severely scarred air sacs (white).
Image courtesy of Dr. Navneet Narula
Stroke, weakened blood vessels, heart damage, neurological deficits—COVID-19 is linked to a long list of complications. Yet perhaps nowhere in the body is the virus’s potentially devastating impact more dramatically illustrated than in the lungs. This dissected sample of a once-healthy lung ravaged beyond repair by the virus is vivid proof. It was taken on March 11, 2021, following a double-lung transplant performed at NYU Langone Health—the third lung transplant for a patient with COVID-19 at the NYU Langone Transplant Institute since December 10, when NYU Langone became the first medical center in New York City to complete a transplant of this type.
A series of whitish spots in the upper and lower lobes indicate widespread scarring around the air sacs, which impedes the transfer of oxygen to the bloodstream. The lung’s outer surface is rough and inflamed, limiting the organ’s ability to expand upon inhalation. Although not visible in this image, the removed lungs were dotted with air-filled cysts, or pneumatoceles, that commonly occur in patients who experience acute respiratory distress and are often a marker of dead tissue. “There’s no normal part of this lung,” says Navneet Narula, MD, professor of pathology at NYU Grossman School of Medicine. “The virus has completely destroyed it.”
The patient, Robert Fernandez Guevara, a 47-year-old man from the Bronx, was infected during the peak of the first wave last spring and admitted to NYU Langone on April 2, 2020, with shortness of breath, a cough, fever, and fatigue. His condition was severe enough to require not only a ventilator, but also a form of life support called extracorporeal membrane oxygenation, or ECMO. It serves as a mechanical gas exchanger that pumps oxygen into the blood while filtering out excess carbon dioxide, a function his lungs were no longer able to perform. The interventions saved Guevara, who was in the hospital for nearly seven months, but his only hope of long-term survival was a new pair of lungs. He was placed on the wait list for an organ donor in January and, just two weeks after the surgery, was discharged, feeling healthy and grateful. “He is doing fantastic,” says Luis F. Angel, MD, professor of medicine and medical director of NYU Langone’s Lung Transplant Program, who marveled as his patient confidently strolled the halls of Rusk Rehabilitation at Tisch Hospital.
A double-lung transplant for COVID-19 is daunting but ultimately curative. The operation can take up to 10 hours—roughly twice as long as a typical lung transplant—because the damaged lungs must be painstakingly separated from the chest wall, the diaphragm, and surrounding tissue, explains Stephanie H. Chang, MD, surgical director of the Lung Transplant Program.
“The rate of lung transplantation for COVID-19 is going to increase,” Dr. Chang predicts, “because of the traumatic lung changes among patients with severe cases of the virus, whether it’s short-term or five years from now.”
NYU Langone is well equipped for the trend. It has completed more than 100 lung transplants since early 2018, a national record for the first 3 years of a program. Most of those cases were for pulmonary fibrosis, a progressive disease that causes lung scarring; emphysema, which occurs when the air sacs are systemically damaged; and cystic fibrosis, an inherited disease that causes thick mucus to form in the lungs, blocking and scarring the airways. The program has the shortest wait time for a donor organ and the highest one-year survival rate in the Northeast, according to data from the Scientific Registry of Transplant Patients.
“We work diligently to get our patients evaluated and listed promptly,” says Dr. Angel. “Our excellent survival rate results from our selection process, our donor management, and the efforts of our multidisciplinary team to monitor patients, some of whom are extremely sick, very closely.”