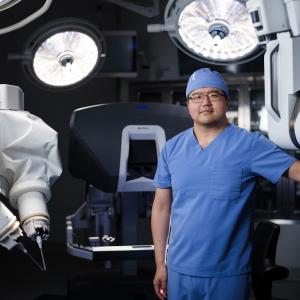
Vascular surgeon Dr. Thomas Maldonado and the Division of Vascular and Endovascular Surgery are studying the safety and efficacy of transcarotid artery revascularization (TCAR), a new and less invasive treatment for patients with carotid artery disease.
Photo: NYU Langone Staff
NYU Langone Health has been at the forefront of innovation in carotid artery disease for four decades—instrumental in advancing surgical techniques for carotid endarterectomy (CEA), as well as contributing to the development of transfemoral carotid stenting. More recently, the medical center has emerged as a leader in a new, minimally invasive procedure: transcarotid artery revascularization (TCAR).
A Promising Alternative
The gold standard treatment for carotid artery disease, CEA, has an excellent record of safety and efficacy, but potential complications include myocardial infarction and cranial nerve injury. The procedure is also contraindicated in certain patients exhibiting advanced age, medical comorbidities, anatomical anomalies, and other factors.
For those patients, transfemoral carotid stenting has been the only alternative. However, this option carries a higher risk of stroke—the very affliction it is intended to prevent. This occurs, in part, because transfemoral carotid stenting requires pushing a catheter through the aortic arch, where plaque often accumulates. Moreover, microemboli dislodged from the carotid artery during stent insertion may elude filters inserted distally to trap debris.
In 2015, the U.S. Food and Drug Administration (FDA) approved TCAR as another option for patients at heightened risk of complications from CEA.
In this procedure, a hybrid of surgical and endovascular techniques, the surgeon makes a small incision just above the clavicle. A specialized sheath is placed directly into the carotid artery and connected to a system that reverses the flow of blood away from the brain to protect against procedural emboli. Meanwhile, the sheath delivers balloon angioplasty and a conformable stent, which stabilizes plaque against the wall of the artery, minimizing potential for a future stroke.
Post-Approval Studies Show Strong Early Results
Preliminary post-approval data for TCAR was presented at the 2019 Society for Vascular Surgery (SVS) annual meeting. In the FDA-mandated ROADSTER 2 trial, TCAR provided a 30-day stroke/death/myocardial infarction rate of 1.7 percent, comparable with rates reported for CEA. In the TCAR Surveillance Project, part of the SVS Vascular Quality Initiative, one study found TCAR associated with lower in-hospital risks of myocardial infarction and cranial nerve injury than CEA, and with similarly low incidence of stroke. Patients also were less likely to need more than a one-day hospital stay.
Another TCAR Surveillance Project study demonstrated lower rates of in-hospital stroke, death, and stroke/death/myocardial infarction with TCAR versus transfemoral carotid stenting in patients 80 and older. Also, lower death rates from all causes were reported in younger patients.
“Like transfemoral stenting, TCAR involves less ischemic time, less recovery time, and less scarring than open surgery,” explains NYU Langone’s Thomas Maldonado, MD, the Schwartz Buckley Professor of Surgery in the Department of Surgery and co-director of the Aortic Disease Center. “And by avoiding the aortic arch and using flow reversal, TCAR offers superior neuroprotection to the transfemoral approach. We believe this technique may become the preferred alternative for high-risk patients.”
NYU Langone Achieves Recognition as a Leading Center for TCAR
Since launching its TCAR program in 2017, NYU Langone has performed more than 50 cases, making it the highest-volume practice in New York City—a distinction reflecting NYU Langone’s status as one of the few academic medical centers in which carotid artery disease is largely managed by endovascular-trained vascular surgeons. The TCAR team is made up of Dr. Maldonado; Glenn R. Jacobowitz, MD, the Frank J. Veith, MD, Professor of Vascular and Endovascular Surgery and chief of the Division of Vascular and Endovascular Surgery; Neal S. Cayne, MD, professor of surgery and director of endovascular surgery; Patrick J. Lamparello, MD, associate professor of surgery; Karan Garg, MD, clinical assistant professor of surgery; and Michael E. Barfield, MD, clinical assistant professor of surgery. The group reports a procedural success rate of 100 percent, surpassing the 97.9 percent rate reported in the ROADSTER 2 post-approval trial.
In August 2019, NYU Langone became the first medical center in New York City to be named a Center of Excellence in TCAR. The designation was awarded by TCAR developer Silk Road Medical, Inc., in recognition of NYU Langone’s leadership in patient volume, record of successful outcomes, and commitment to ongoing research in the technique.
Seeking an Even Safer Way Forward
NYU Langone is also pursuing research aimed at improving outcomes with TCAR. In 2019, investigators, led by Dr. Maldonado, submitted a paper for publication detailing ways surgeons can avoid certain low-frequency but significant errors such as traumatic dissection of a bovine arch. In addition, Dr. Maldonado launched a study investigating differences in patients’ ability to tolerate reversal of blood flow during TCAR surgery.
“The question we’re exploring with both of these studies is, ‘How can we make an exceptionally safe procedure even safer?’” Dr. Maldonado says. For the blood flow study, he and his colleagues will explore why approximately 1 percent of TCAR patients—those who have the procedure under local anesthetic—lose consciousness when flow is reversed. Strikingly, this number is far lower than the 10 to 12 percent who respond similarly when the common carotid artery is clamped during CEA and who must be shunted to protect against ischemic stroke.
The team plans to test for biomarkers, such as neuron-specific enolase and sp100, that might help explain the differences in patient response. The biomarkers also may help predict which individuals will do best with which procedure.