Analysis by NYU Langone Researchers Settles Decades-Long Debate Over Value of Newer Drug Class
Angiotensin receptor blockers (ARBs) are as effective as angiotensin converting enzyme (ACE) inhibitors developed 10 years earlier despite previous study results to the contrary, according to an analysis by researchers at NYU Langone Medical Center. Their findings are the result of a meta-analysis of more than 100 published clinical trials of both drugs and were published online this month in the journal Mayo Clinic Proceedings.
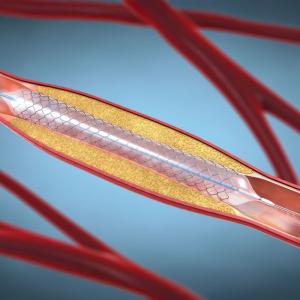
The two classes of drugs, ACE inhibitors and ARBs, interfere in different ways with the function of angiotensin II, a hormone that regulates blood pressure. As part of the body’s response to low blood pressure, the hormone restricts flow through blood vessels to raise the pressure. ACE inhibitors prevent the synthesis of angiotensin II, while ARBs prevent the hormone from passing on its message by taking its place in protein receptors on blood vessel surfaces.
“There has been debate for many years over the safety and efficacy of ACE inhibitors compared to ARBs, with many of them using an 'ACE inhibitor-first' approach, with ARBs regarded as less effective,” says Sripal Bangalore, MD, an associate professor in NYU Langone’s Leon H. Charney Division of Cardiology, Department of Medicine, and lead study author. “We believe that our study ends the debate and gives physicians the option to prescribe either drug for their patients.”
VIDEO: Dr. Sripal Bangalore discusses the differences between the blood pressure medications angiotensin receptor blockers (ARBs) and angiotensin converting enzyme (ACE) inhibitors.
Previous analysis had concluded that ACE inhibitors were more effective than ARBs for treating hypertension. Dr. Bangalore says that this difference is due to a “generation gap” between the two sets of trials. According to Dr. Bangalore, early trials of ACE inhibitors showed a clear benefit when compared to placebo, but ARB trials done a decade later did not show as pronounced a benefit over placebo. Part of that difference may be explained by changes in the standard of care over the decade between the trials. Patients in the later ARB trials benefited from a greater emphasis on smoking cessation and statin use along with the study drug, making its effect seem smaller compared to placebo than during the ACE inhibitor trials era, when those strategies were not as commonplace.
Thus, previous meta-analysis of the two drugs by other researchers that found that ACE inhibitors should be “first-line therapy” to reduce mortality were based on indirect inferences, not head-to-head, randomized clinical trials, and should be reconsidered, Dr. Bangalore says.
The results of the current meta-analysis showed that outcomes for ACE inhibitors and ARBs compared to placebo were similar when trials were done at similar time points. The only difference was that the ARBs were better tolerated. These results were then confirmed in head-to-head comparison trials where there were no significant differences except for better ARB tolerability.
Specifically, the current research team conducted a meta-analysis of 106 randomized trials that enrolled 254,301 patients. The selected trials compared ACE inhibitors or ARBs to placebo, and were conducted after 2000 to better account for the generation gap between the two medications, such as improvements in patient background risk, including statin use and smoking cessation.
“This is the first time that we have a clear and consistent message from the three buckets of trials of ACE inhibitors and ARBs all of which show that there is not outcome difference between the two agents except for better tolerability of ARBs,” says Dr. Bangalore.
“The results of our analysis,” Dr. Bangalore adds, “are especially important for patients given that many ARBs are now also generic, which reduces their costs.”
Dr. Bangalore’s co-authors were Robert Fakheri, MD, Gbenga Ogedegbe, MD, and Howard Weintraub, MD, of NYU Langone Medical Center; Bora Toklu, MD, of Mount Sinai Beth Israel; and Franz H. Messerli, MD, of University Hospital, Bern, Switzerland and the Icahn School of Medicine at Mount Sinai.
Media Inquiries
Allison Clair
Phone: 212-404-3753
allison.clair@nyumc.org