Photo: rightdx/Getty
Certain patients with an aggressive form of ovarian cancer have a better chance of a cure through surgical removal of the tumor before chemotherapy instead of the reverse, a new study shows.
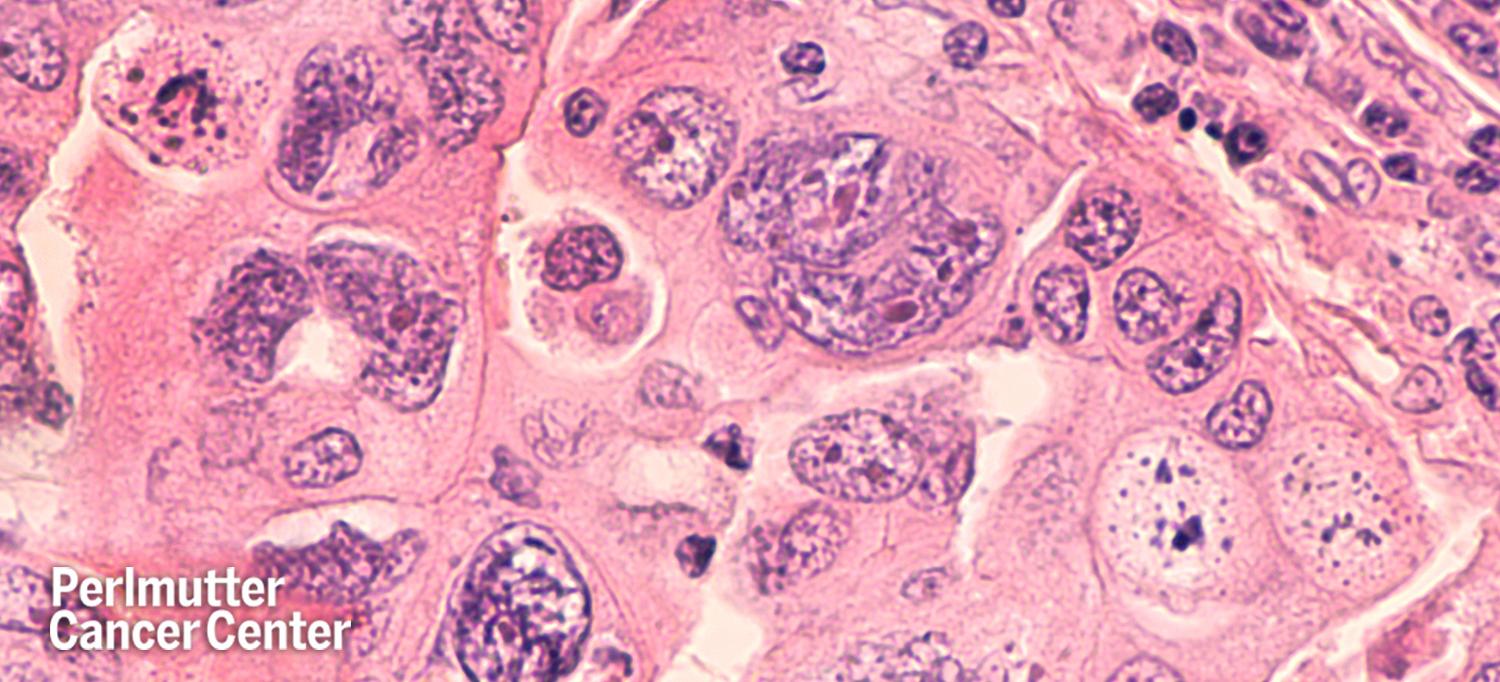
Led by researchers at NYU Langone’s Perlmutter Cancer Center and Dana-Farber Cancer Institute, the study used a mathematical tool to examine how doctors should coordinate available treatments for high-grade serous ovarian cancer (HGSC).
Ovarian cancer is the eighth most common cancer and a major cause of cancer death in women worldwide, and HGSC constitutes roughly 70 percent of ovarian malignancies and has the worst prognosis. Patients with the condition typically have surgery and chemotherapy, but there has been long-standing controversy over the best order of treatment.
Published online June 14 in Proceedings of the National Academy of Sciences, the new analysis argues that patients who can have “complete debulking” surgery first, with chemotherapy added after (termed primary debulking surgery or PDS), should have a superior outcome to the other main treatment option: giving patients a few cycles of chemotherapy to shrink the tumor before surgery (neoadjuvant chemotherapy, or NACT).
“The issue of whether PDS or NACT should be used was highly controversial, and a major reason for it lies in the different characteristics of patients in different clinical studies,” says study first author Shengqing Gu, PhD, a graduate from University of Toronto and now an instructor at Dana-Farber Cancer Institute. “We therefore built a mathematical model to simulate HGSC clinical course, which allows us to compare treatment outcomes in the same virtual patients and examine which group of patients may respond differently to PDS versus NACT.”
“Our model, combined with earlier clinical data, suggests that for patients who can undergo complete debulking, surgery offers the best chance of long-term survival or even cure,” says study co-senior author Benjamin G. Neel, MD, PhD, director of NYU Langone’s Perlmutter Cancer Center. “Our model also provides some insight about optimal early detection and treatment intervals.”
The researchers used clinical data from roughly 300 patients in previous studies of patients’ responses to PDS or NACT, taken from the Princess Margaret Cancer Center in Toronto and the Canadian Cancer Trials Group.
The researchers found that in patients who are well enough for surgery, debulking provides better results because it has the best chance of removing cancer cells resistant to chemotherapy. For patients who are too ill for debulking surgery, the study suggests that a shorter period of initial chemotherapy, rather than the currently recommended interval, might provide a greater benefit.
The current analyses suggest several questions that future randomized clinical trials should examine, say the study authors. These include how much the influence of the time gap between surgery and subsequent chemotherapy may affect treatment outcome, whether there is a link between the number of initial chemotherapy cycles and outcomes, and whether complete secondary surgery on relapsed tumor improves prognosis.
“Our model shows that a fraction of patients can have long-term survival or even cure, but only when they undergo complete debulking, followed by the currently available therapies,” Dr. Neel says. “There is an urgent need for new therapies to provide cures for patients for whom complete debulking is not an option and for those with the most treatment-resistant cancer cells.”
This study was supported by National Institutes of Health (NIH) grants R37 49152, R01 257507, and P30 CA008748; the NIH Terry Fox Foundation (TFPPG 721 020003), the Mary Kay Foundation, DCA Award from University of Toronto and Sara Elizabeth O’Brien Trust Fellowship, Ontario Ministry of Health and Long Term Care, and the Princess Margaret Cancer Foundation.
Along with Dr. Neel, the co-corresponding author for this study is Myles Brown at Dana-Farber Cancer Institute. Other authors are Stephanie Lheureux, Azin Sayad, Paulina Cybulska, Liat Hogen, Iryna Vyarvelska, Marcus Bernardini, Barry Rosen, and Amit Oza at Princess Margaret Cancer Center in Toronto; Dongsheng Tu and Wendy Parulekar at Canadian Cancer Trials Group; Matthew Nankivell at University College London; Sean Kehoe at University of Birmingham, United Kingdom; and Dennis Chi at Memorial Sloan Kettering Cancer Center and Weill Cornell Medicine.
Dr. Neel is a co-founder, holds equity in, and received consulting fees from Navire Pharma, Northern Biologics, Inc, and Jengu Therapeutics, Inc. He also receives consulting fees and equity from Arvinas, Inc., has equity in Recursion Pharma, received consulting fees from MPM Capital, and was an expert witness for the Johnson & Johnson ovarian cancer talc litigation in U.S. Federal Court. His spouse has or held equity in Amgen, Inc., Regeneron, Moderna, Inc., Gilead Sciences, Inc., and Arvinas, Inc. These relationships are being managed in accordance with the policies of New York University.
Media Inquiries
Greg Williams
Phone: 212-404-3500
gregory.williams@nyulangone.org

