Urologist Dr. Lee C. Zhao brings complexities into focus with his new research study highlighting the need for pre-counseling and careful follow-up to increase positive outcomes for masculinizing genital reconstructive surgery.
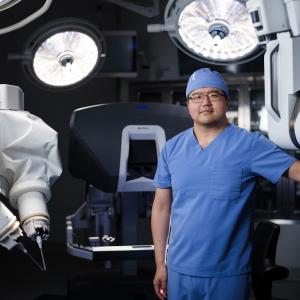
Photo: NYU Langone Staff
Patient demand for gender-affirming surgery—including facial, chest, and genital reconstructive surgery (GRS)—has increased in recent years and become more accessible due to changes in insurance coverage. However, only a handful of institutions worldwide offer these complex operations. A recent study led by NYU Langone’s Lee C. Zhao, MD, assistant professor in the Department of Urology, suggests that many patients receive the initial surgery far from home and seek follow-up care for short-term complications with other surgeons.
Complications Emerge Soon After Surgery
In a retrospective study published online June 20, 2019, in Urology, Dr. Zhao, who is also director of male reconstructive surgery and co-director of transgender reconstructive surgery—part of NYU Langone’s transgender surgery services—and colleagues report on the cases of 55 patients who experienced urethral complications following masculinizing GRS.
All patients, who ranged in age from 17 to 60, sought care with one of the study’s 8 co-authors a median of 4 months following their initial surgery at a different center. Anastomotic stricture was the most common form of urethral complication, occurring in 66 percent of patients. Most patients presented with 2 or more complications, the authors note, and all of those with urethrocutaneous fistula (56 percent) had concurrent urethral stricture.
The findings underscore a scenario that is becoming increasingly common and often challenging for reconstructive urologists—the expectation of managing complications stemming from procedures at other centers. The urologist may lack important details about the original operation, and patients may be surprised or confused about the need for additional interventions.
“Urethral complications after masculinizing genital surgery is very different from urethral strictures occurring in cisgender patients after trauma,” Dr. Zhao says. “The techniques needed to revise these strictures are different, and even when the operative reports are available, there is no substitute for the knowledge of the anatomy that the original surgeon had.”
Patient Counseling and Access to Care Are Critical
Urethral complications are common following masculinizing GRS, with published rates from 25 to 75 percent, according to Dr. Zhao. However, due to geographic and cost constraints, many patients may have difficulty following up with their primary surgeons even during the immediate postoperative period.
“It’s important to counsel patients that the risk of postsurgical complications is highest in the first few months following surgery,” Dr. Zhao says. “Patients should be made aware that they should follow up closely with the surgeon who performed the surgery. While care with a reconstructive urologist is certainly helpful, like for any other complex surgical procedure, there is no substitute for follow-up with the surgeon who performed the surgery.”
“At NYU Langone, we have a high-volume practice in gender-affirming surgery, with patients traveling from all over the world for care. One thing that we stress before scheduling any surgery is the expectation for the patient to return to New York for postoperative care.”
A Broad Range of Complications
“Masculinizing genital reconstructive surgery, especially phalloplasty, involves a number of separate operations: vaginectomy, perineoplasty, urethroplasty, scrotoplasty, and radial forearm free flap,” Dr. Zhao says. “Each of these procedures have complications. When all of these procedures are performed simultaneously, it is natural for complications to add up.”
The variety of surgical techniques used by the co-authors highlights the broad range of potential urethral complications following masculinization surgery, as well as the lack of standardized approaches to address them.
For example, patients who received multiple prior skin grafts for urethral repairs had fewer options for reconstruction. In addition, almost half of the patients presented with vaginal remnant. This can occur after the primary vaginectomy if the mucosa is incompletely resected, leaving remnants in the urinary tract. Patients may experience symptoms including difficulty voiding, leakage, pain, and recurrent urinary tract infections.
“Treatment of vaginal remnants typically requires complete excision and closure of associated tracts,” says Dr. Zhao. “At NYU Langone, we remove the vaginal remnant via a robotic approach. Since the patients previously had a perineal reconstruction, we are able to avoid making an incision into the perineum to completely remove the vaginal remnant.”
A Program Built on Continuous Quality Improvement
“Due to the complexity of the operation and the unacceptably high rate of complications, it makes sense to have a constant process of quality improvement. At NYU Langone, we perform both revision surgery and primary gender-affirming surgery. Taking care of complications from other centers has really informed how we perform the primary operation,” Dr. Zhao says. “We’ve found that complications often lead to other complications, such as urethral strictures causing urethral fistula or wound breakdown. Thus, we perform phalloplasty in stages to prevent one complication from causing others.”
The authors caution that the study is limited by its small size and incomplete details from institutions where the primary surgeries were performed. However, the findings highlight the importance of alerting patients to the signs and symptoms of complications and of having access to long-term follow-up care.
“In addition to reconstructive urologists who are prepared to evaluate and treat patients with complex surgical needs,” Dr. Zhao says, “this study highlights the need for thorough preoperative counseling and long-term local follow-up of transgender patients who undergo masculinizing GRS,” concludes Dr. Zhao.