Herbert Lepor, MD
PHOTO: Jay Brady
The NYU Langone Health radical prostatectomy prospective database is one of few enabling long-term longitudinal tracking of post-prostatectomy survival and quality of life outcomes. New findings offer encouraging news for men who are considering or who have undergone radical prostatectomy to treat prostate cancer.
Incontinence May Develop as Part of Aging
Despite surgical advances, the development of urinary incontinence following open and robotic radical prostatectomy remains a feared limitation of the treatment. In 2004, Herbert Lepor, MD, professor of urology and biochemistry and molecular pharmacology and the Martin Spatz Chair of Urology, and colleagues reported that 97 percent of men undergoing radical prostatectomy regained urinary continence within two years. A recent review of long-term patient data led by Dr. Lepor, presented at the 2017 Asia-Pacific Prostate Cancer Conference in Melbourne, Australia, revealed that over a period of 15 years, urinary continence rates declined to 89.8 percent. These 15-year incontinence rates were independent of age at the time of surgery, suggesting that men of all ages should be counseled that incontinence may develop years after the surgical procedure.
Prospective studies from Scandinavia have indeed demonstrated that as they age men in the general population are at risk of developing urinary incontinence as a result of bladder outlet obstruction from the enlarging prostate. According to Dr. Lepor, while radical prostatectomy may cause urinary incontinence by compromising sphincter function, removing the malignant prostate prevents urinary incontinence that would have developed from the benign enlargement of the prostate.
Prostate Removal May Protect against Some Urinary Symptoms
Nearly all men—from 25 percent of 40-year-olds to 90 percent of 80-year-olds—experience some benign prostatic hyperplasia (BPH) as they age. Although prior studies have shown that many men experience worsening urinary symptoms due to BPH over time, the long-term prospective outcomes study shows this does not occur in men who have undergone radical prostatectomy.
Approximately 40 percent of men have moderate to severe lower urinary tract symptoms (LUTS) immediately prior to undergoing radical prostatectomy. Following radical prostatectomy, these men will experience marked symptom improvement, which is durable over 15 years. Of the men who have mild LUTS immediately prior to undergoing radical prostatectomy, very few develop progressive and bothersome LUTS. The annual cost of managing BPH is approximately $4 billion in the United States alone. Radical prostatectomy appears to alleviate the economic burden and adverse quality of life impact of BPH.
Focal Ablation and Active Surveillance May Control Prostate Cancer
Organ-sparing surgery for prostate cancer has the potential to circumvent the side effects of radical prostatectomy, but whether it would control disease has been unclear, since prostate cancer is typically multifocal. A team led by Dr. Lepor has recently demonstrated that in select patients, focal ablation may achieve an acceptable level of disease control when paired with careful postsurgical monitoring.
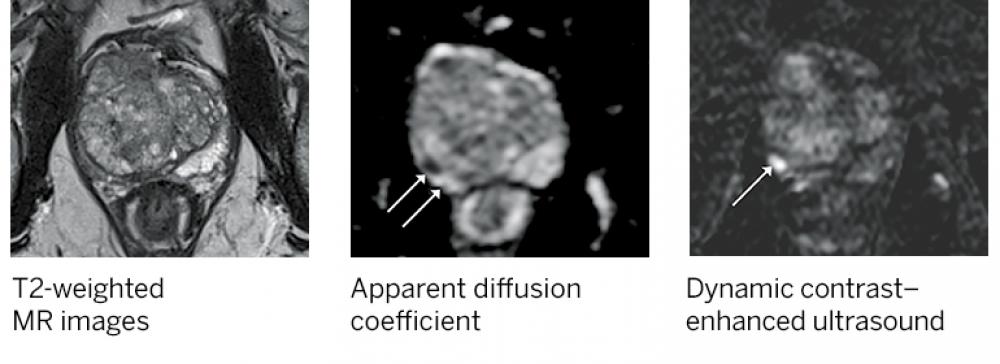
The study, published online in Urology in October 2017, relied on rigorous MRI-guided prostate mapping to identify 59 men who were candidates for focal ablation but chose radical prostatectomy between 2012 and 2016. The criteria included a single reported MRI lesion concordant with a biopsy Gleason score (GS) less than eight, no gross extraprostatic extension on MRI, no GS above six or six with a core length greater than five millimeters contralateral to the reported MRI lesion.
Reviewing postsurgical radical prostatectomy specimens, the investigative team concluded that 43 (72.9 percent) harbored multifocal disease. In addition, the MRI correctly identified the pathological index lesion, defined by the highest GS and tumor volume, in 55 of 59 cases (93.2 percent), reinforcing the value of MRI in identifying the disease that drives the biology of the cancer. The researchers concluded that focal ablation would have eradicated all Gleason pattern 4 disease in most cases and that any remaining Gleason pattern 4 extrafocal disease would have been very low volume. The potential for recurrent disease necessitates ongoing active surveillance, both within and outside the treatment zone.
“Skeptics of focal ablation should remember that more than half of men whose low-risk disease is managed with active surveillance have undiagnosed Gleason pattern 4 disease,” says Dr. Lepor. “Ultimately, the efficacy of focal ablation will need to be confirmed through randomized control studies comparing it with other treatment options,” he adds.
NYU Langone and its Perlmutter Cancer Center, recognized as a center of excellence for image-guided detection and focal ablation, will play an instrumental role in defining candidates for focal ablation and optimizing oncological and functional outcomes following this novel approach to treating prostate cancer.