Gastroenterologist Dr. Seth A. Gross and colorectal surgeon Dr. Mitchell A. Bernstein collaborate to bring their individual expertise to patients with gastrointestinal cancers.
Photo: Karsten Moran
NYU Langone Health gastroenterologists and surgeons are at the forefront of using robotics and artificial intelligence (AI) to detect and treat gastrointestinal cancers. The collaborative members of the multidisciplinary team bring together their expertise in advanced endoscopy and minimally invasive colorectal surgery to deliver the best possible treatment to patients.
Flexible Robotic Scope Offers Alternative to Surgery
Seth A. Gross, MD, associate professor in the Department of Medicine and director of clinical care and quality in the Division of Gastroenterology and Hepatology, and Mitchell A. Bernstein, MD, professor in the Department of Surgery and director of colorectal surgery, were among the first doctors in the country to use the new endoscopic Flex Robotic System (Medrobotics) in the gastrointestinal tract. Using a robotic platform, the team removed a large premalignant rectal lesion in a patient who was discharged home the same day.
The procedure involves inserting a flexible scope into the anus while the patient is under general anesthesia. Using a robotic console, physicians snake the illuminated endoscope to the site of the lesion, where a high-definition, three-dimensional camera provides a clear view of the patient’s anatomy. “The flexible robotic scope gives us the ability to work effectively in a very tight space,” says Dr. Gross. “The articulating arms of the robot allow us to perform surgical techniques from an endoscopic point of view.”
Physicians navigate the robotic scope to a position in front of the target lesion and then dock it to establish a stable platform, says Dr. Gross. The procedure instruments are then inserted down the side ports until they become visible in front of the camera.
“The flexible robotic scope gives us the ability to work effectively in a very tight space,” says Dr. Gross. “The articulating arms of the robot allow us to perform surgical techniques from an endoscopic point of view.”
“The technique is particularly effective for removing large precancerous lesions in the lower colon,” Dr. Gross explains. “These lesions are challenging to remove using conventional colonoscopy and traditionally may require abdominal surgery.”
This flexible system is also being used to treat rectal cancer, says Dr. Bernstein. For example, NYU Langone surgeons are using it in transanal total mesorectal excisions (TMEs), which involve excising the anus through the rectum rather than cutting through the pelvis. The flexible scope overcomes the limitations of laparoscopic instruments, which are difficult to maneuver in the narrow confines of the pelvis, adds Dr. Bernstein. “We are one of the very few centers doing transanal TME to treat rectal cancers,” he says. “The flex scope offers an exciting new platform that promises to enhance our ability to perform this innovative technique and improve patient care.”
AI-Assisted Colonoscopy
Physicians are also evaluating emerging AI tools to enhance detection of potentially cancerous lesions, says Dr. Gross. The use of computer programs loaded with tens of thousands of images of normal and diseased colons enhances conventional endoscopic procedures. Dr. Gross is a co-investigator in one of the first studies exploring whether real-time AI can help find polyps not just in a computer lab but in patients undergoing colonoscopy.
Before beginning an AI-assisted colonoscopy, Dr. Gross plugs his monitor into an AI-enabled computer. As he scans the patient’s colon, the computer flags regions with potential abnormalities that merit further investigation.
“AI gives us an extra pair of eyes,” says Dr. Gross. “It has the specificity and sensitivity to allow us to do a better surface inspection of the colon compared with conventional methods.”
The long-term potential for AI-enhanced procedures extends well beyond colonoscopy, Dr. Gross adds. For example, it might be used to better target areas with potentially precancerous changes for biopsy in patients at high risk of developing cancers of the gastrointestinal tract, such as those diagnosed with ulcerative colitis or Barrett’s esophagus.
“The AI-assisted technology offers great promise for enhancing the quality of our screening and diagnostic procedures, especially in the detection of precancerous and cancerous lesions,” says Dr. Gross.
Expanding Treatment Options for Patients
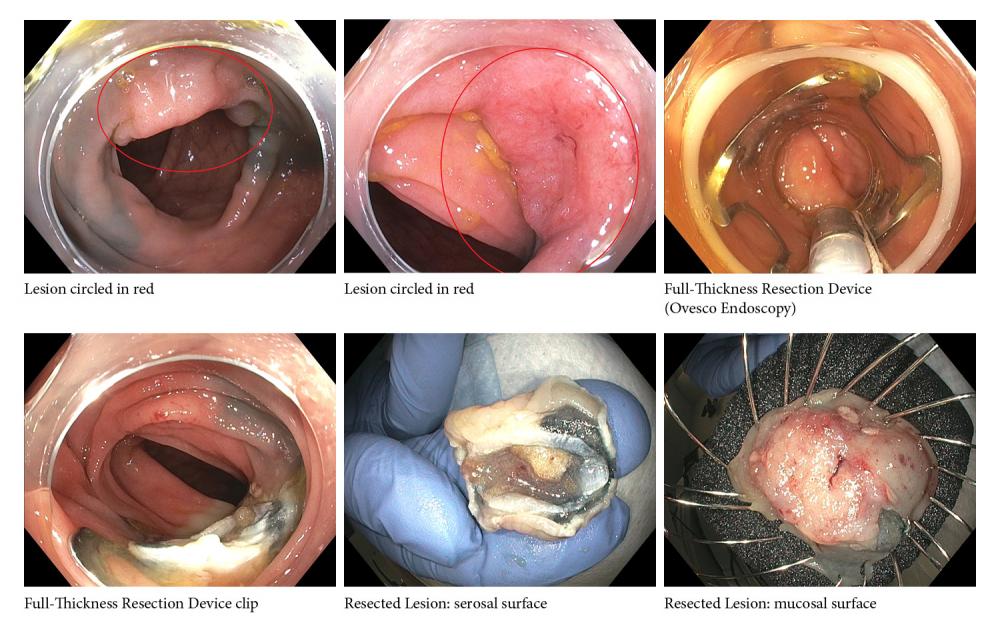
Gregory B. Haber, MD, professor in the Department of Medicine, chief of endoscopy and director of advanced therapeutics and innovation in the Division of Gastroenterology and Hepatology, is a pioneer in performing full-thickness bowel resections with a novel endoscopic device that may be needed for lesions that are deeply rooted or in hard-to-reach locations.
Program faculty are crafting minimally invasive approaches to treating conditions that have traditionally required surgery, he says. Currently, 10 percent to 20 percent of colon resections performed are for premalignant but still benign polyps. With advances in endoscopic resection, Dr. Haber and his team hope to reduce the number of unnecessary surgeries for these benign lesions.
Furthermore, early cancers detected in the mucosa or the superficial submucosa can now be cured with endoscopic techniques such as full-thickness resection performed at routine colonoscopy on an outpatient basis, with patients immediately returning to normal diet and activity.
An advance in the palliative management of malignant obstructions of the stomach, which previously had to be accomplished with surgery, is the use of endoscopic ultrasound guidance to access the gastrointestinal tract, says Dr. Haber. Using endoscopic ultrasound techniques, physicians can place a uniquely designed lumen-apposing metal stent across the stomach wall directly into the jejunum to provide drainage of the obstructed stomach.
The new ultrasound-guided therapeutic applications are expanding to include drainage of organs which are inaccessible to luminal endoscopy. Not only can we perform endoscopic gastro-jejunostomies, we are able to replace percutaneous gallbladder drainage with a totally internal drainage with function-specific stents to create cholecysto-duodenostomies.
“Our ultimate aim is to be able to do more and more procedures with a minimally invasive approach so we can individualize care and provide the most appropriate options for each patient,” says Dr. Haber. “Close collaboration with our colleagues in surgery and interventional radiology is critical to achieving that goal.”
A Commitment to Education: Advanced Endoscopy Fellowship Program
Furthering its commitment to cultivating the next generation of specialists, NYU Langone has introduced an advanced endoscopy fellowship program under the direction of Lauren G. Khanna, MD, program director and assistant professor in the Department of Medicine, and Dr. Haber. The program accepts two fellows each year and provides multisite experience with broad exposure to advanced procedures; participation in national society meetings, presentations, and clinical trials; and participation in training junior fellows.