Photo: Callista Images/Getty
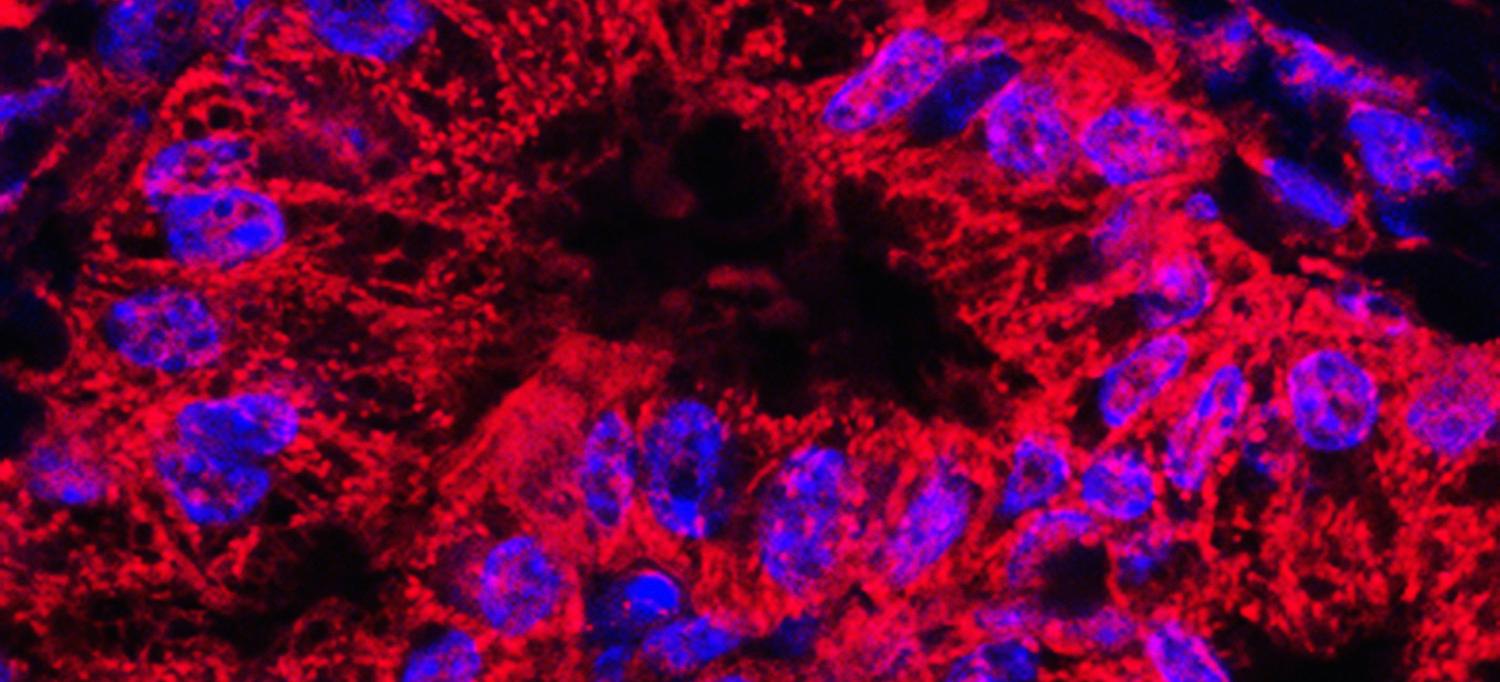
Pancreatic cancer cells avert starvation by signaling to nerves, which grow into dense tumors and secrete nutrients. This is the finding of a study with experiments in cancer cells, mice, and human tissue samples published online November 2 in Cell.
The study addresses pancreatic ductal adenocarcinoma (PDAC), the deadliest cancer of the pancreas with a 5-year survival rate below 10 percent. Such tumors encourage the growth of dense tissue that presses on blood vessels, reducing the supply of blood-borne nutrients like serine. This amino acid is used as a building block for proteins, and is required for cancer cells to multiply.
Led by researchers from NYU Grossman School of Medicine, the Department of Radiation Oncology at NYU Langone Health, and Perlmutter Cancer Center, the new study found that starving pancreatic cancer cells secrete a protein called nerve growth factor (NGF), which sends signals for extensions of nerve cells, instructing them to grow deeply into tumors. The researchers found further that such extensions, called axons, secrete serine, which rescues pancreatic cancer cells from starvation and restores their growth.
“Our study offers more proof that pancreatic cancers are remarkable metabolic scavengers, which contributes to their deadliness,” says corresponding author Alec Kimmelman, MD, PhD, the Anita Steckler and Joseph Steckler Chair of the Department of Radiation Oncology at NYU Langone. “The ability of nerves to funnel nutrients from the bloodstream to the more austere pancreatic tumor microenvironment is a fascinating adaptation, and could lead to therapeutic approaches that interfere with this unique flexibility.”
The study found that pancreatic cancer cells starved of serine take advantage of the process by which messenger RNA (mRNA) strands, copies of DNA instructions, are translated into proteins. Backbones of mRNA molecular strands, called bases, are decoded into amino acids using three-base units called codons. Cellular machines called ribosomes read each codon as they link amino acids together in the right order, but ribosomes stall if there is a lack of available amino acids.
Surprisingly, the research team found that serine-starved pancreatic cancer cells more significantly slow the rate at which two of the six serine codons (TCC and TCT), but not all six as assumed, are translated into amino acid chains. Under serine-starved situations, this variability lets cancer cells minimize the production of certain proteins (to preserve energy stores during starvation), but continue to build stress-adaptive proteins like NGF, which happens to be encoded by few TCC and TCT codons.
NGF and other factors are known to encourage nerves to grow into pancreatic tumors, and to increase tumor growth as well. The current study is the first to show that axons, extensions of neuronal cells that transmit their signals, provide metabolic support to cancer cells by secreting serine in nutrient-deprived areas, say the authors.
The new publication is one of many by Perlmutter Cancer Center researchers in recent years that describes the ways in which pancreatic cancer cells find energy. A 2016 study revealed that such cells send signals to nearby stellate cells, causing them to break down their own cell parts into building blocks that can be used by tumors. Then a December 2019 study found that pancreatic cancer cells also hijack a process called macropinocytosis, which normal cells use to pull nutrients in through their outer membranes. Interestingly, the new work found that stellate cells and macropinocytosis cannot supply enough serine for these cancer cells to grow, and that axonal delivery is required.
In a glimpse of potential future applications for the study, mice with PDAC tumors fed serine-free diets saw 50 percent slower tumor growth. To go beyond what diet alone could achieve, the researchers also blocked the recruitment of axons into PDAC tumors using a drug already approved by U.S. Food and Drug Administration called LOXO-101. The drug blocks the activation of a receptor protein on the surface of neurons that interacts with NGF (also called TRK-A), thereby inhibiting the ability of neurons to send their axons into tumors.
The drug alone did not slow PDAC tumor growth in mice, say the authors, but slowed it by an additional 50 percent when combined with a serine-free diet, compared with the diet alone. This suggests that nerves were necessary to support PDAC cell growth in serine-deprived regions of the tumor, researchers say.
“As TRK inhibitors are approved in the treatment of some cancers, they might have value in combination with a low-serine diet following surgery in the perhaps 40 percent of patients with PDAC tumors that can’t make serine,” says lead study author Robert Banh, a postdoctoral scholar in Dr. Kimmelman’s lab. “Whether this approach could decrease tumor recurrence by limiting the nutrient supply would need to be confirmed in clinical trials.”
Along with Dr. Kimmelman and Dr. Banh, study authors from NYU Langone Health and Perlmutter Cancer Center are Douglas Biancur; Keisuke Yamamoto; Albert Sohn; Beth Walters; Robert J. Schneider, PhD; and Michael E. Pacold, MD, PhD. Also authors are Miljan Kuljanin, Ajami Gikandi, and Joseph Mancias of the Division of Genomic Stability and DNA Repair, Department of Radiation Oncology, at Dana-Farber Cancer Institute in Boston; along with Huamin Wang of the Department of Anatomical Pathology at MD Anderson Cancer Center in Houston.
The study was funded by the Damon Runyon Cancer Research Foundation (DRG-2348-18) and by National Institutes of Health grants T32 CA009161, F99 CA245822, 1K22CA212059, R01CA157490, R01CA188048, P01CA117969, R35CA232124, R01GM095567, T32 CA9161-41, and R01CA178509. Also supporting the work were a Uehara Memorial Foundation Research Fellowship, a Mary Kay Foundation Cancer Research Grant (017-32), the Shifrin-Myers Breast Cancer Discovery Fund at NYU, a V Scholar Grant funded by the Hearst Foundation (V2017-004), American Cancer Society grant RSG-13-298-01, the Lustgarten Foundation, Stand Up to Cancer (SU2C), Breast Cancer Research Foundation grant BCRF-16-143, the Burroughs Wellcome Fund Career Award for Medical Scientists, the Farber Cancer Institute Claudia Adams Barr Program for Innovative Cancer Research Award, and the Hale Family Center for Pancreatic Cancer Research.
Dr. Pacold reports having options in Raze Therapeutics and receiving travel funds from Thermo Fisher Scientific. Dr. Kimmelman reports have financial interests in Vescor Therapeutics, LLC, and having consulting relationships with Rafael/Cornerstone Pharma and Deciphera Pharma. All relationships are being managed in accordance with the policies of NYU Langone.
Media Inquiries
Greg Williams
Phone: 212-404-3500
gregory.williams@nyulangone.org

