Gastroenterologist Dr. Abraham R. Khan and surgeon Dr. Tanuja Damani collaborate to bring their expertise to patients at the Center for Esophageal Health.
Photo: NYU Langone Staff
Recently, a patient at NYU Langone’s multidisciplinary Center for Esophageal Health presented with an unusual case of achalasia with concurrent gastroesophageal reflux disease (GERD) and hiatal hernia.
The patient was a 71-year-old woman with a longstanding history of heartburn, which responded to treatment with a proton pump inhibitor. However, the patient’s sensation of dysphagia, which she described as “food feels stuck,” had been going on for several years, rendering her unable to enjoy meals. The patient’s sensation of obstruction, characteristic of esophageal dysphagia, had progressively worsened over the years. Subsequently, she noted additional symptoms of increasing cough and hoarseness.
Diagnosis and Relief Remain Elusive with Traditional Testing
Diagnostic testing at another institution included conventional esophageal manometry and a barium esophagram, used to assess esophageal emptying and the morphology of the gastroesophageal (GE) junction. In this case, the esophagram suggested an esophageal stricture, a complication of GERD usually found in proximity to the GE junction.
Upper endoscopy excluded neoplasm as the cause of dysphagia. Esophageal dilation of the stricture, performed during endoscopy, did not result in improving the patient’s symptoms.
Achalasia was suggested, but not confirmed, by subsequent high-resolution esophageal manometry, a more sensitive test for diagnosing achalasia compared with conventional manometry. Achalasia, a rare neuromuscular disorder affecting the esophagus, affects about only 1 to 3 per 100,000 people per year.
Patient Referred to NYU Langone for Advanced Diagnostic Testing
The patient’s out-of-state physician referred her to Tanuja Damani, MD, surgical director of the Center for Esophageal Health. As with other complex cases, Dr. Damani conferred with Abraham R. Khan, MD, the center’s medical director. The diagnosis was not certain when the patient met with Dr. Khan, who specializes in neurogastroenterology and motility disorders of the gastrointestinal (GI) tract.
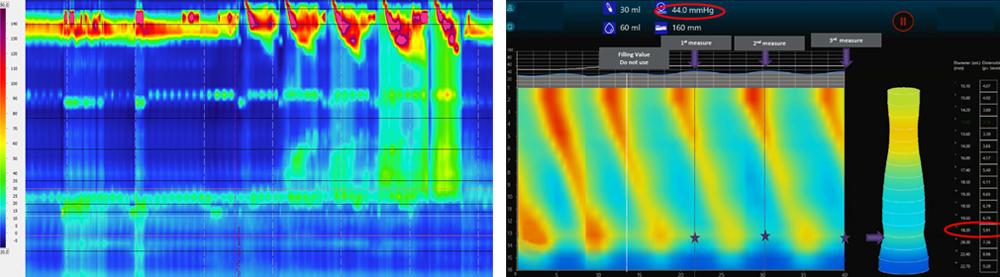
After thoroughly reviewing and analyzing the patient’s history and previous diagnostic test results, Dr. Khan, assistant professor in the Department of Medicine within the Division of Gastroenterology and Hepatology, suggested advanced diagnostic testing with careful interpretation. The patient underwent endoscopy with a functional lumen imaging probe (FLIP), which revealed likely achalasia. FLIP technology uses high-resolution impedance planimetry during volume-controlled distension to measure luminal pressure and geometry, assess the mechanical properties of the esophageal wall, and evaluate the opening dynamics of the GE junction. Repeated high-resolution esophageal manometry was performed under a specialized protocol to include solid food and rapid drink challenges.
Careful analysis by Dr. Khan confirmed the likelihood of achalasia as the underlying physiology causing the difficulty in swallowing. When interpreted in total, the tests also confirmed the patient’s persistent GERD physiology with a hiatal hernia, which rarely occurs concurrent with achalasia.
Teamwork Leads to Successful Planning and Resolution of Conditions
Collaborative planning by a team with broad shared expertise in esophageal gastroenterology and foregut surgery led to a decision to proceed with a robotic Heller myotomy. This surgery widened the lower esophageal sphincter by cutting individual muscle fibers of the esophagus. Dr. Damani, assistant professor in the Department of Surgery, also accomplished concurrent robotic repair of the hiatal hernia with a Toupet fundoplication as an antireflux procedure.
The patient recovered rapidly and was discharged after 36 hours. She required no pain medications, as the surgery had been performed using minimally invasive techniques, with quarter-inch incisions. The patient continues to do well, reporting complete resolution of dysphagia and significant improvement of GERD symptoms.