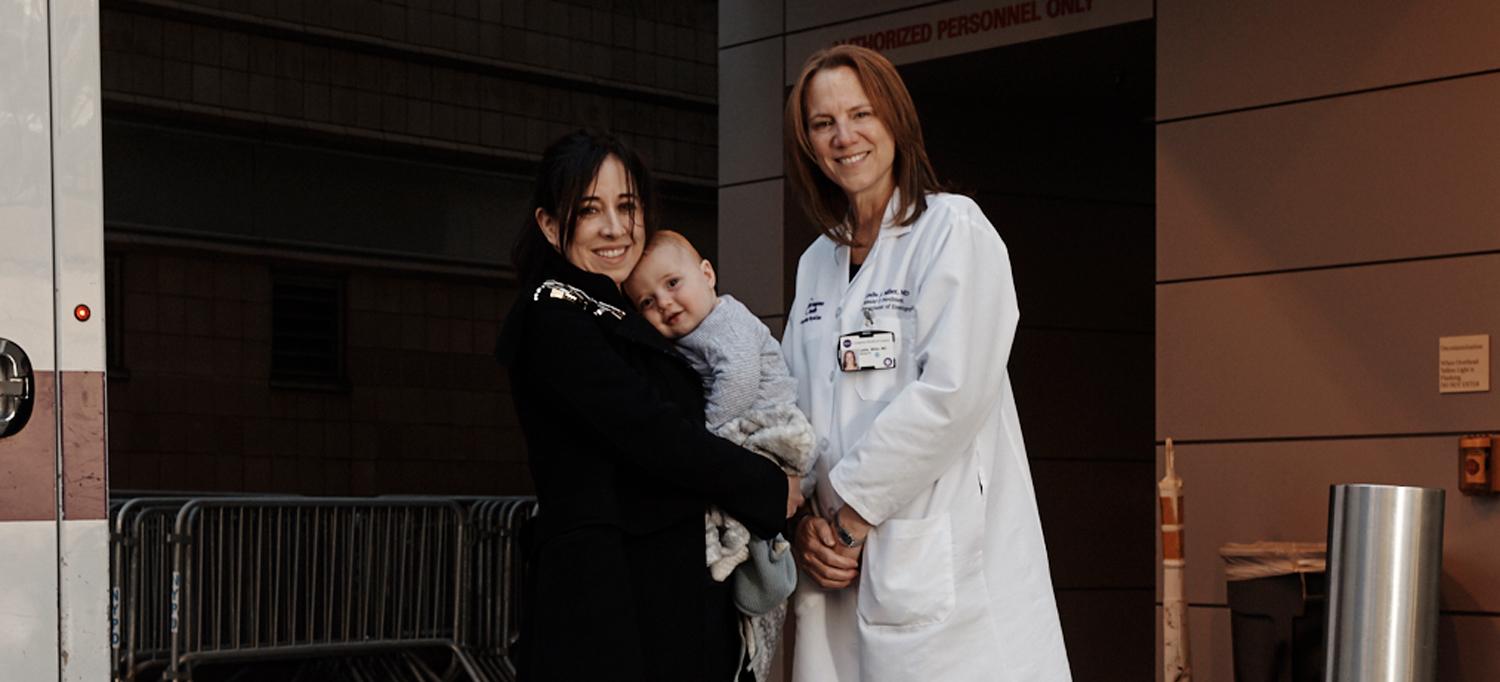
Tammy Fried introduces Dr. Leslie Miller to her son, Max, outside the emergency department where her dramatic journey began.
Photo: Tony Luong
Like many people, Tammy Fried was skeptical about the value of a video visit with a doctor. When she awakened one morning in May 2020 with a nosebleed and bloody cough, she was concerned about her symptoms but wondered what a doctor could possibly do for her over the phone. Still, Fried, then seven months pregnant, was reluctant to make a trip to the emergency department amid the coronavirus disease (COVID-19) pandemic. So instead, she made an appointment with NYU Langone Health’s Virtual Urgent Care service, as thousands of patients had done throughout the spring surge.
Fried, a tax attorney who lives on Manhattan’s Upper West Side, soon found out just how valuable NYU Langone’s telemedicine service could be. Her outreach marked the first step of a long, complex medical journey in which a team of NYU Langone specialists drew upon its wide-ranging expertise and keen decision-making to save her life.
It all began with Leslie J. Miller, MD, an emergency medicine physician with 30 years of experience, who fielded Fried’s Virtual Urgent Care visit last May. “With pregnancy, one of the things you have to be very concerned about is spontaneous bleeding,” explains Dr. Miller, clinical associate professor of emergency medicine. It’s not uncommon for people to cough up blood due to pneumonia, bronchitis, or other respiratory conditions, she notes. But Dr. Miller could hear Fried’s cough sounding progressively wetter, suggesting an increasing amount of blood in her lungs. Sensing that her condition was deteriorating, Dr. Miller explained the need for a CT scan to help diagnose a potential vascular abnormality. “You need to go to the emergency department,” she told Fried. “The sooner, the better.”
Soon after Fried arrived at the Ronald O. Perelman Center for Emergency Services at NYU Langone’s Tisch Hospital, she was coughing up an alarming amount of blood. Concerned that an underlying disorder was causing Fried to hemorrhage, doctors ordered a CT scan, expedited by Tina S. Wu, MD, MBA, clinical associate professor of emergency medicine. The scan didn’t show evidence of a life-threatening blood clot known as a pulmonary embolism, nor did it identify the cause of the bleeding. The same was true for an endoscopy of Fried’s airway, which ruled out a severe nosebleed as the culprit. With Fried stabilized in the emergency department, Dr. Wu transferred her to the intensive care unit. There, she was sedated and intubated, and a bronchoscopy was performed to remove blood from her lungs and identify the location of the bleeding.
“By isolating the source of the bleeding, the bronchoscopy helped us correlate what we would see on an angiogram,” explains Akhilesh K. Sista, MD, chief of the Division of Vascular and Interventional Radiology at NYU Langone. Using the angiogram’s series of X-rays to view the integrity of the blood vessels, Beatriz Escobar, MD, clinical assistant professor of radiology, was able to identify the precise source of the bleeding. A fistula, or abnormal connection between two blood vessels that are normally excluded from one another, had formed between the bronchial and pulmonary arteries. Upon bursting, it had caused blood to leak into Fried’s lungs—slowly at first, and then with greater force. Through a pinhole incision in the groin, Dr. Escobar threaded a catheter to the bronchial artery, but she was unable to block it off because one of the microwires damaged blood vessels, which sometimes occurs during the procedure. “This is a very unusual place for a fistula to form,” notes Dr. Sista, “and it can be very challenging to gently guide a wire through a tortuous vessel.”
Fried continued to cough up small amounts of blood over the next few days, which were suctioned out by the intensive care team. When the vessels healed several days later, Dr. Sista, the interventional radiologist on duty, was able to successfully block off the artery by plugging it with metallic coils, which prevented blood from spilling into Fried’s lungs. Dr. Sista describes this embolization technique as one of the most advanced procedures performed by interventional radiologists, placing NYU Langone at the forefront of the field. “Anytime there’s internal bleeding,” he says, “we can employ high-end mechanical and imaging technology to plug it up, avoiding major surgery.”
Her bleeding issue resolved, Fried and her baby faced a new threat. She had developed a severe form of preeclampsia, a life-threatening condition that affects multiple organ systems, including the mother’s liver and kidneys. When it became clear that Fried’s organ damage was worsening, maternal–fetal medicine specialist Sara G. Brubaker, MD, MPH, clinical assistant professor of obstetrics and gynecology, recommended delivery, which reverses the complications of the illness. Though Fried was frail from 10 days of hospitalization, 8 spent on a ventilator, her baby was strong at just 30 weeks of gestation. On May 26, five days after being weaned off sedation, Fried gave birth via cesarean delivery to a 3-pound 15-ounce boy. “To hear the baby cry,” she says, “was like hearing the angels sing. It felt like everything was going to be okay.” After 10 weeks in the Neonatal Intensive Care Unit at Tisch Hospital, “Miracle Max,” as his parents referred to him, went home to meet his 3-year-old brother, Jack.
“Twenty years ago, people used to say that emergency departments were a safety net for patients,” notes Dr. Miller. “But COVID-19 has made telemedicine another safety net.” When Fried made a full recovery, she sent Dr. Miller a note to thank her for the expert care she provided during their video visit. “You saved my life,” she wrote.
Fried recently had a chance to thank Dr. Miller and Dr. Sista in person, during a meeting arranged by the TODAY show.
Watch more from TODAY.

