Joshua S. Silverman, MD, PhD, and Douglas Kondziolka, MD
PHOTO: Karsten Moran
Ongoing research continues to uncover and enhance the efficacy of Gamma Knife® radiosurgery for an expanding array of conditions, including cancer and arteriovenous malformations (AVMs). Aided by enhanced surveillance, physicians at the Center for Advanced Radiosurgery are tracking and targeting tumors more precisely and employing Gamma Knife’s versatility to treat conditions previously considered untreatable, improving options and outcomes for the most complex cases. The approach is illustrated by two recent, very different cases in which Gamma Knife radiosurgery’s precision proved invaluable: the successful treatment of a patient with more than 25 individual tumors and the highly delicate resolution of an otherwise unresectable AVM.
Precision Radiosurgery Combines with Genetically Tailored Drugs to Control Cancer
For cancer patients with brain metastases, conventional whole-brain radiation treatment can result in a host of side effects, including memory impairment, fatigue, hair loss, and reduced independence. With the use of Gamma Knife radiosurgery, a more targeted effective alternative, notes Douglas Kondziolka, MD, the Gray Family Professor of Neurosurgery, professor of radiation oncology, vice chair of clinical research in the Department of Neurosurgery, and director of NYU Langone’s Gamma Knife program, patients can be spared these side effects.
Paradoxically, as systemic treatments improve for various cancers, the incidence of metastases in the brain—less affected by systemic therapies—is increasing, making their targeted treatment more important than ever. In 2017, Dr. Kondziolka and colleagues at NYU Langone published a study in the Journal of Neurosurgery demonstrating tumor control rates near 100 percent for brain tumors less than a centimeter in diameter that had been targeted early. “As the evidence continues to mount and prove the Gamma Knife’s efficacy, more oncologists are surveilling patients and finding brain tumors earlier—enabling us to be more proactive and to avoid neurological symptoms,” says Dr. Kondziolka.
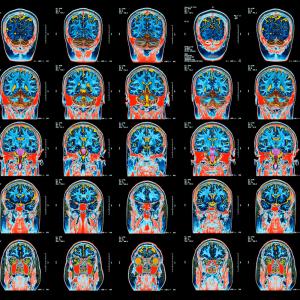
A recent patient provides a case in point. Referred to Dr. Kondziolka for consultation, the patient had been previously diagnosed with, and treated for, lung cancer, which involved a mutation that made it susceptible to a targeted drug treatment. In addition to the lung cancer, the patient was found to have 15 small tumors in his brain. “We used precisely targeted Gamma Knife radiosurgery to destroy all 15 tumors, and the patient responded beautifully,” notes Dr. Kondziolka.
During the next year, the patient’s lung cancer improved with drug treatment, and quarterly brain scans showed he was clear of brain tumors. A year after the initial Gamma Knife treatment, however, 13 new brain tumors appeared. “With quarterly surveillance, we spotted them early, when they were still small,” says Dr. Kondziolka, “and at that size, we expected these new tumors to respond very well again.”
As before, Dr. Kondziolka’s team treated the 13 tumors with the Gamma Knife and the patient continued on drug therapy. A year later—two years after the patient’s first brain cancer diagnosis—he remains active and without symptoms, which Dr. Kondziolka attributes in part to the effective genetically targeted lung cancer treatment and in part to the early detection and successful radiosurgery of the brain tumors that did occur.
Although tumors could recur, notes Dr. Kondziolka, that has not happened, and the patient maintains perfect neurological function. “Patients like these are breaking the ‘rules’ of cancer,” he adds.
Gamma Knife Surgery for an “Unresectable” AVM
Treatment of AVMs in the brainstem always presents a clinical challenge because of the region’s many critical neurologic functions, but in many cases the Gamma Knife has proved to be a critical tool in their treatment. In 2017, the NYU Langone radiosurgery team co-authored a series of publications—two that appeared in the journal Neurosurgery and a third in World Neurosurgery—highlighting multicenter studies of Gamma Knife surgery outcomes for AVMs in the brain, all affirming the surgery’s efficacy for patients less suitable for resection or curative embolization.
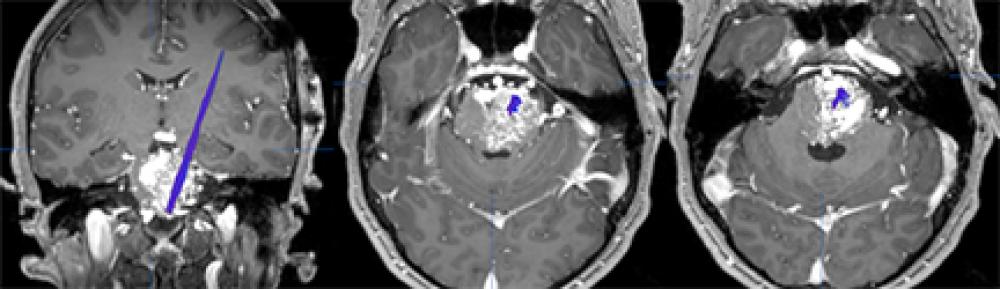
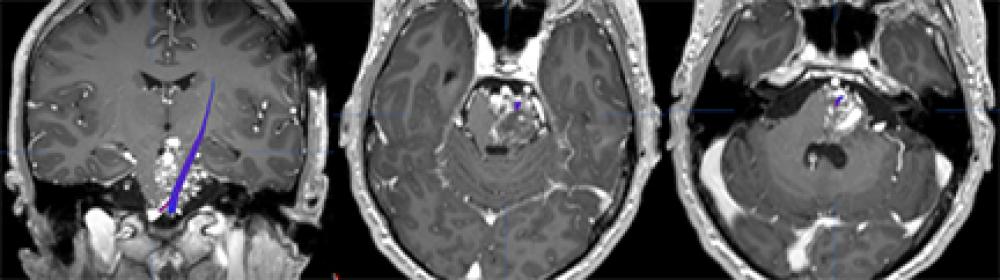
For some patients with highly complex AVMs, the Gamma Knife provides a surgical option when traditional resection is ruled out. One such patient presented to Dr. Kondziolka more than five years ago with a congenital brainstem AVM so complex, it was thought to be untreatable. The whole brainstem looked like a massive collection of blood vessels, requiring a very thoughtful treatment approach. “At that time, nobody knew what to do—you could never have cut it out,” notes Dr. Kondziolka. “Because of its complexity, we decided not to touch this AVM.” Several years later, that plan became untenable, when the AVM hemorrhaged and caused a stroke. “At this point, we had to do something,” continues Dr. Kondziolka. “I talked to colleagues around the country, and we decided to attempt a very careful treatment approach using the Gamma Knife.”
In collaboration with NYU Langone’s neuroradiologists, the team employed diffusion tensor imaging during the procedure to visualize the brainstem nerve fiber tracts. Then, to avoid injuring the nerve fibers, they used a small amount of Gamma Knife energy to target the AVM. “It was a very precise use of the technology,” notes Dr. Kondziolka. A year later, the patient is doing well. “The AVM looks like it’s closing off, the patient’s motor tracts are fine, and he is an active young man,” says Dr. Kondziolka. “This patient experienced an excellent outcome for what was thought to be an unresectable condition,” he says. “We’re seeing more and more cases where Gamma Knife changes the trajectory of treatment, ultimately delivering a positive outcome.”