Dr. Babak Givi and Dr. Michael Persky discuss outcomes data following the Department of Otolaryngology—Head and Neck Surgery’s monthly quality improvement patient safety conference.
Photo: Karsten Moran
With a shift in culture designed to emphasize individual performance improvement and collective safety enhancements, the multidisciplinary team within the Department of Otolaryngology—Head and Neck Surgery is using data-driven insights to home in on opportunities to enhance quality. As efforts to reduce surgical risks improve outcomes, NYU Langone’s otolaryngologists are pushing forward with newer, more sophisticated reconstruction approaches that enhance patients’ quality of life.
Transparency Across the Surgical Team
An emphasis on transparency has emerged from a department-wide focus on quality in three key areas: structure, process, and outcomes. Improvement across each area demands a shared dedication to quality enhancements based on transparent data and metrics. “We’re applying new analyses to our data over time to acknowledge patterns, demonstrate cause and effect, and push quality forward,” notes J. Thomas Roland Jr., MD, the Mendik Foundation Professor of Otolaryngology and chair of the Department of Otolaryngology—Head and Neck Surgery.
Quality improvement begins with the surgical team itself, who are all fellowship-trained surgeons who prioritize quality and safety, especially as more patients undergo increasingly complex procedures. Detailed procedure data reveal insights such as individual complication rates, duration of surgery, and total procedure costs. These real-time insights then inform conversations targeting performance improvements. “I’ll say, ‘Why does this surgery take twice as long for you,’ or ‘Do you know if you have had any postoperative hemorrhage?’” explains Dr. Roland. “Accurate data yield honest, realistic conversations aimed at improving what we do so we’re as safe, reliable, and efficient as possible.”
These data can also lead to process improvements such as reduction in unnecessary doses of antibiotics and pain medications. A continuous feedback loop helps department leaders monitor changes in protocol, keep close track of high-risk patients, and flag complications that arise, such as readmissions. Outcomes are reviewed during the monthly quality improvement patient safety conference, where trends are identified and solutions outlined to align standard protocols with the prevention of complications. “We look at each case completed over the past month and key outcomes indicators—returns to the OR, infection rate, length of stay—to find readily adoptable ways to improve outcomes and lower costs,” adds Dr. Roland.
In keeping with the institution-wide adoption of high-reliability organization (HRO) principles, these efforts extend to every member of the multidisciplinary team, including nurses, who are empowered to voice concerns when an aspect of care fails to measure up. Nurses can encourage surgeons to return to an anxious patient’s room, for example, to review discharge instructions or remind other members of the team of best practices in infection prevention.
Safety and Volume Increase in Tandem
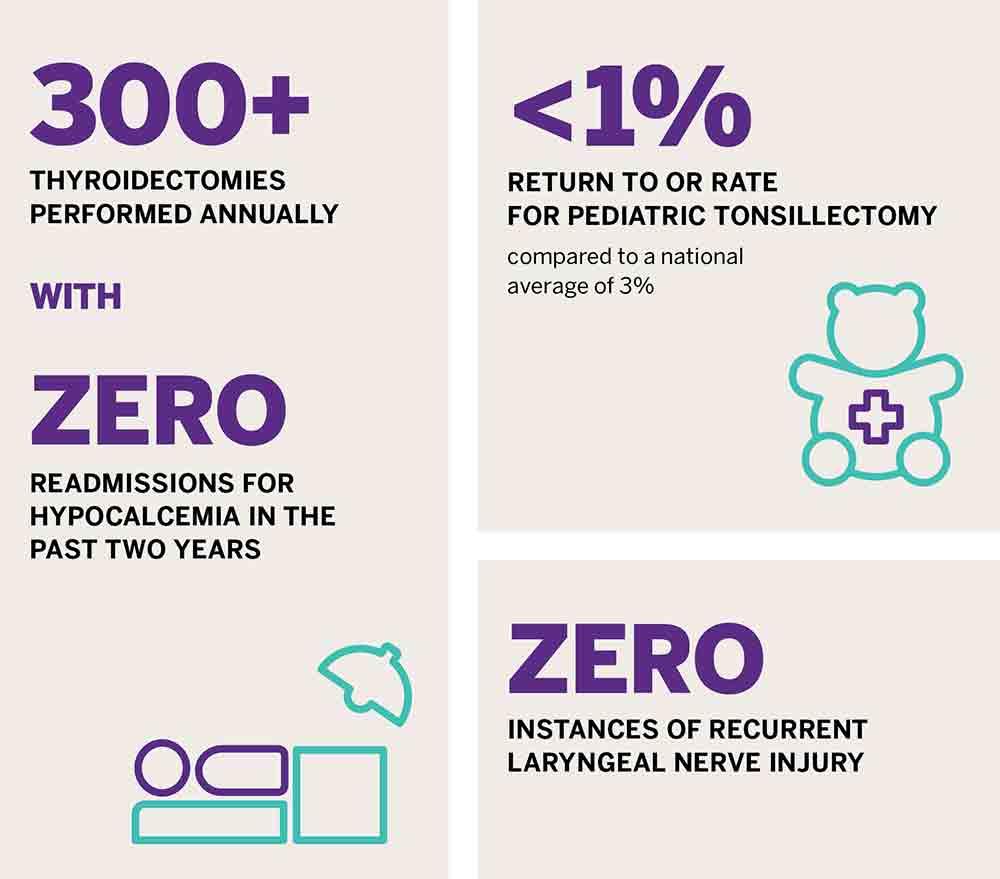
The focused quality improvement efforts across the department have had a measurable impact on patient safety metrics, which indicate complication rates that fall below specialty-wide published rates. This trend is observed across the high-volume procedures performed by department surgeons, including high-volume pediatric tonsillectomy, which shows an operating room (OR) return rate of less than 1 percent at NYU Langone versus a national average of 3 percent.
Thyroidectomy is another high-volume procedure, with research presented at the Triological Society in 2018 pointing to a national average readmission rate due to hypocalcemia of 4 percent 30 days after the procedure. At NYU Langone, the rate has been 0 for the past 2 years—even with the high thyroidectomy volume in the Division of Head and Neck Surgery averaging around 300 procedures per year. A similar 0 rate is observed for recurrent laryngeal nerve injury, a devastating complication that was previously documented nationally at 1 to 5 percent. “The message to patients is, ‘If you come to NYU Langone, your risk of having major complications is almost zero,’” notes Babak Givi, MD, associate professor of otolaryngology—head and neck surgery.
Maintaining a consistently low rate of complications is enabled through new techniques and approaches that emerge from the department’s monthly quality improvement patient safety conferences. One unique approach: highlighting prospective, rather than retrospective, data around adverse events. “Everyone at the table can see that we did 400 operations in a month with a 0.3 percent readmission rate, and every care deviation or complication that occurred,” says Dr. Roland. “So we’re all aligned in understanding variations in quality and making adjustments to our individual and collective approaches as needed.”
Quality Begets Quality
With surgical risk contained, specialists in the department are poised to reexamine long-held practices and identify approaches to raise care quality further still—even as they offer patients increasingly complex reconstruction techniques that more closely restore their pre-disease conditions. Focused initiatives include analyzing the department’s antibiotic use, paring back their prophylactic use and duration in certain low-risk patients. “We looked at the data and saw that we had zero infection or return rates for thyroidectomy—so we said, ‘Let’s try reducing the number of antibiotics we’re giving, perhaps without warrant,’” says Adam S. Jacobson, MD, associate professor of otolaryngology—head and neck surgery and co-director of the Head and Neck Center.
A similar approach in multidisciplinary management has been taken with the Department of Radiology and Division of Hematology and Medical Oncology to implement thyroid function monitoring following head and neck radiation. The initiative has resulted in a notable improvement in performance, published in 2019 in The Laryngoscope. Inspiration for further projects often comes from otolaryngologists-in-training, a third of whom must be involved in quality improvement projects. “They’re on the front lines and often the first to recognize opportunities to do better in terms of patient care,” explains Dr. Roland.
Finding Quality Beyond the Data
The department’s reputation for excellence, which draws in complex patients from across the country, is built on more than raw data. An emphasis on interpersonal patient skills is also central to monthly quality reviews. Empathy, transparency, and a proactive approach are critical, says Dr. Roland, especially when inevitable complications occur.
“A patient who’s had post-op facial paralysis—a recognized surgical risk—should become a surgeon’s favorite patient,” he says. “You want to show them the most attention, communicate with them more regularly, and get them into facial rehabilitation sooner. Those patients need all the information and insights you have in order to make good decisions about their care.”