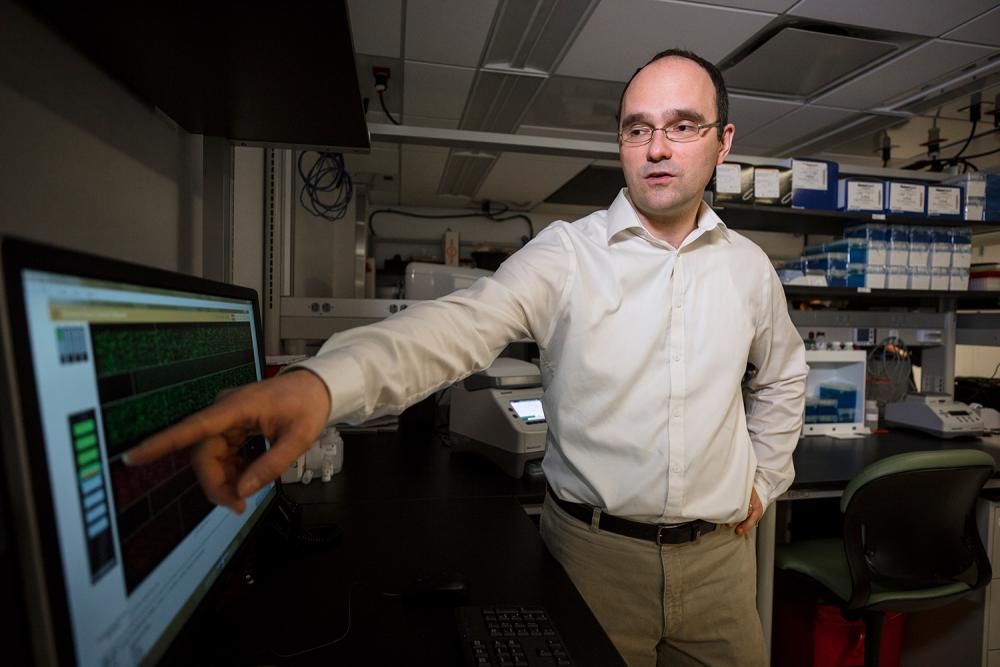
Using laser interstitial thermal therapy (LITT), Dr. Dimitris G. Placantonakis has been able to offer patients a new treatment approach for inoperable brain tumors.
Photo: Juliana Thomas
Clinicians at NYU Langone’s Brain Tumor Center are expanding brain tumor treatment options with a new laser-based ablation approach, while a collaborative effort to develop genetically based cancer screenings is advancing the complementary fields of cancer diagnosis and research.
Laser Ablation Provides Minimally Invasive Option for Intractable Tumors
Laser interstitial thermal therapy (LITT), a tumor ablation technique in use at NYU Langone throughout the past year, offers a new treatment approach to inoperable brain tumors.
Stereotactic navigation guides the placement of an infrared laser probe that heats and destroys the adjacent cancerous tissue, with real-time MRI informing the precise positioning required for this treatment. “This approach gives us tremendous control over the ablation process,” notes Dimitris G. Placantonakis, MD, PhD, assistant professor in the Department of Neurosurgery. “It expands our reserve of treatments in cases that lack surgical options due to tumor location, or when a patient’s age or overall health makes a craniotomy unfeasible.”
The therapy’s application in an 80-year-old patient with a newly diagnosed, otherwise inoperable glioblastoma deep within the brain offered encouraging results. “We decided to use the laser instead of chemotherapy and radiation, which likely would have been ineffective,” notes Dr. Placantonakis. “Nine months later, the patient was, instead, doing very well. I have no doubt this treatment extended his life.”
LITT may also be indicated to counter brain swelling effects from radiation treatment, as a minimally invasive therapy for tumors untreatable with resection or radiosurgery, and for tumors that don’t respond to currently efficacious treatment options.
“In addition to its use for brain tumors, we’re looking at laser ablation as a potential treatment for epilepsy and movement disorders, with clinical trials anticipated here in the near future,” adds Dr. Placantonakis.
Revolutionizing Cancer Diagnostics with Novel Genetic Techniques
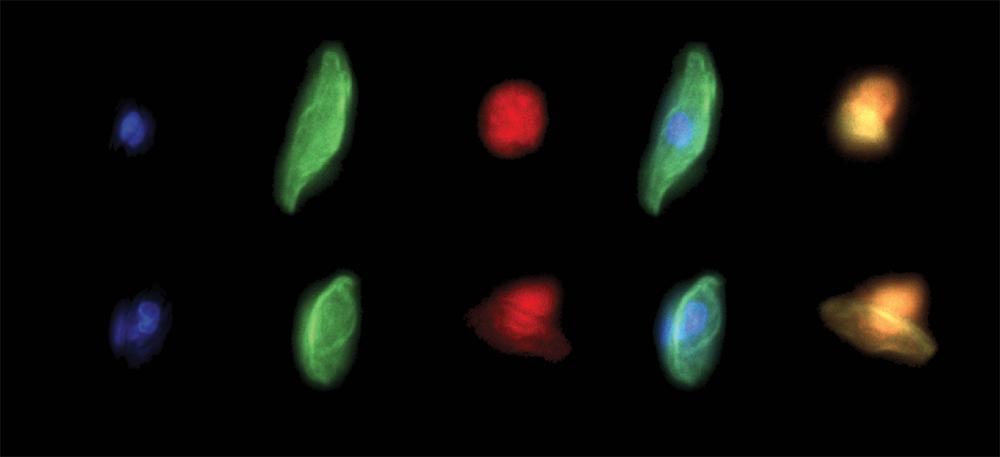
A 580-gene diagnostic panel, resulting from a 2-year collaboration between the Department of Pathology and NYU Langone’s Perlmutter Cancer Center, provides a comprehensive framework for comparing the sequencing results of normal and tumor tissue DNA.
Approved in mid-2018 by the New York State Department of Health, the panel reveals genetic differences that may drive tumor growth, with the goal of informing targeted treatment strategies.
“Our team custom-built the gene panel, selecting genes known to be diagnostic or actionable with FDA-approved drugs, as well as mutations expected to be treatable by drugs on the horizon,” says Matija Snuderl, MD, assistant professor of pathology and director of molecular pathology. “Our goal was to capture as much genetic information as we could from cancers of various origins, because we know that the same mutations—which potentially could be targeted with the same drug—arise with different frequency in cancers throughout the body.”
Dr. Snuderl and his team plan to use the gene panel as a foundation for detailed cancer investigations, with findings then translated into basic science studies that could lead to therapeutic targets.
Eventually, it may be used to screen all cancer patients and offered as a service to regional medical centers that lack such diagnostic resources. “To have our own large sequencing panel that serves as a flagship genomic screening for national institutions represents a new era for NYU Langone,” says Dr. Snuderl.
Two additional novel screenings developed by Brain Tumor Center researchers are now being reviewed for approval by New York State. One, a sequencing panel that looks for nearly 100 specific gene fusions that drive tumor growth, can help to identify treatments for individual cancers; the other examines the DNA methylation profile of brain tumors to identify specific subtypes.
“We plan to be the first certified lab in the United States to use epigenetic profiling and machine learning to diagnose brain cancers,” says Dr. Snuderl. “These screening tools represent important milestones in our efforts to better align brain tumors with their most effective treatments.”
New Expertise Refines Center’s Clinical, Research Emphasis
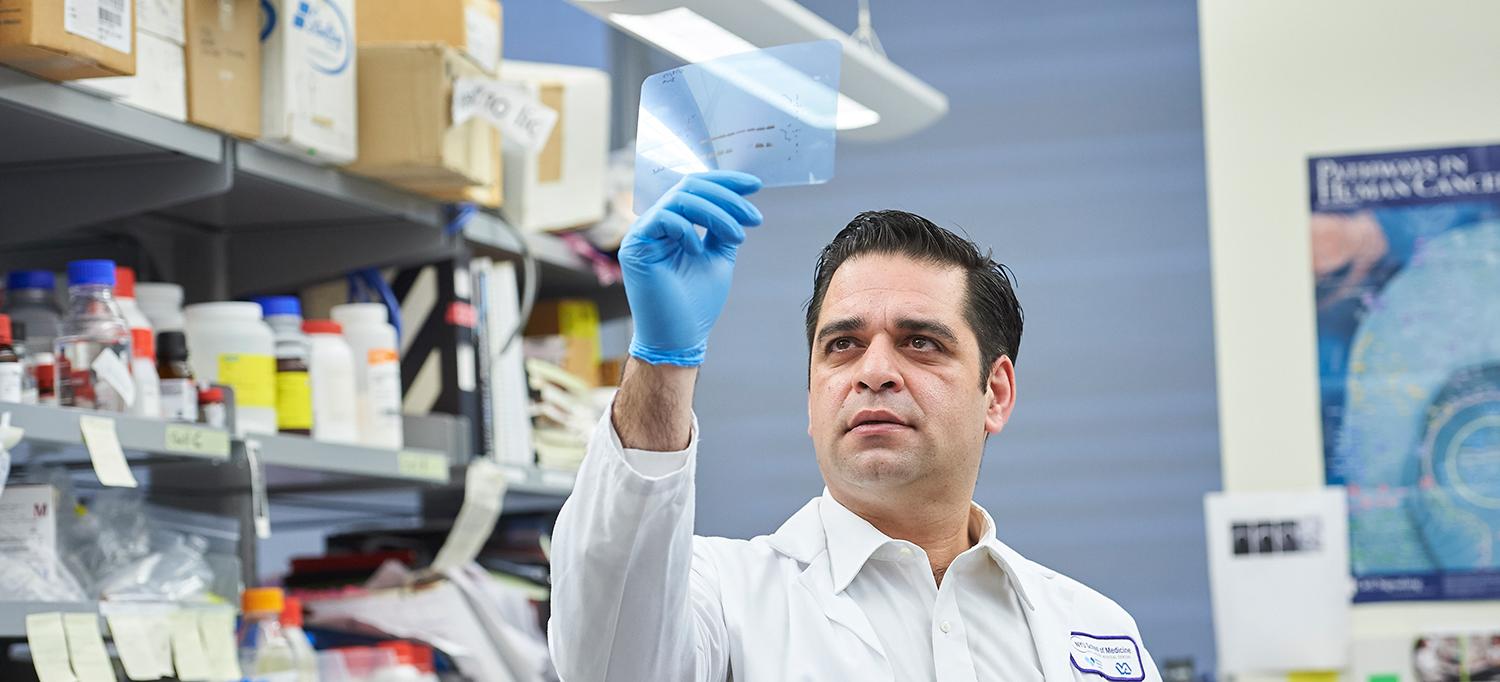
The Brain Tumor Center has reaffirmed its commitment to forward-thinking patient care with the addition of Erik P. Sulman, MD, PhD, co-director of the Brain Tumor Center and vice chair of Research in the Department of Radiation Oncology.
Dr. Sulman brings deep experience combining radiation planning with advanced imaging and immuno-oncology to achieve maximum treatment benefit for patients, expanding the center’s armamentarium of cutting-edge radiation treatment modalities.
Dr. Sulman will adapt the center’s translational research programs to target critical problems associated with brain tumor treatment, such as expanding its investigations into neuropsychological approaches to counter the effects of radiation and chemotherapy.
“It is thought that there may be genetic predictors associated with these neurocognitive effects,” he explains. “Exploring these factors [enables us] to align our laboratory research with our clinical focus.”
Traditionally, therapeutic outcomes have been emphasized, notes Dr. Sulman, but the goal at NYU Langone is to round out the patient experience with multidisciplinary services, including psychiatric care, rehabilitative medicine, integrative medicine, and palliative care. “The idea is to address the overall brain health of the patient with a combined approach focused on both tumor control and patient wellbeing,” he says.