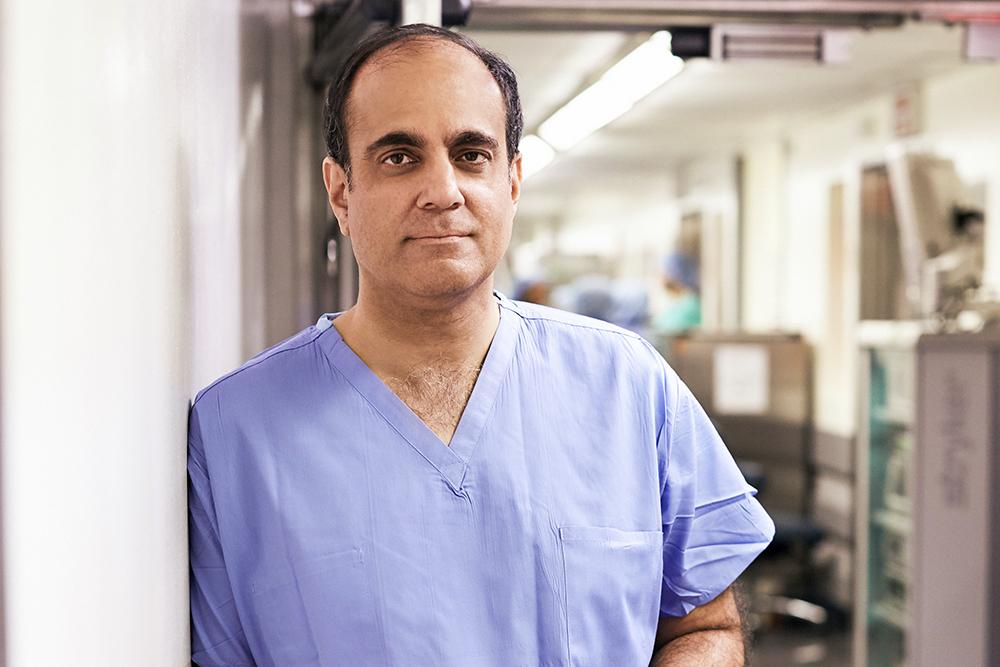
Dr. Herbert Lepor and other urologists conduct research on focal ablation, a prostate cancer treatment that results in fewer side effects.
Photo: Karsten Moran
To meet the challenges of treating prostate cancer while reducing associated risks, NYU Langone continues to lead research identifying new applications for focal ablation (FA). This promising, minimally invasive alternative to radical prostatectomy and radiation therapy causes fewer treatment-related complications and may be the optimal management choice for a select group of men with clinically localized prostate cancer.
Research Homes in on Optimal Focal Ablation Candidates
Optimal management of the spectrum of prostate cancers includes a range of options, from active surveillance to whole-gland removal. In select cases, recent research points to focal ablation (FA) as a viable alternative that can potentially control disease while preserving the patient’s quality of life, says Herbert Lepor, MD, professor in the Departments of Urology and Biochemistry and Molecular Pharmacology, and the Martin Spatz Chair of Urology.
The studies have found that FA not only achieves acceptable disease control in select patients, but also results in far fewer of the treatment-related complications—such as urinary, gastrointestinal, and sexual side effects—that frequently accompany radical prostatectomy or radiation therapy.
Selecting candidates for FA is based on detecting lesions with MRI. MRI does not detect very small, low-risk disease, but it has been shown to identify the index (or most aggressive) tumors accurately in 93 percent of candidates for FA who underwent radical prostatectomy, according to one study led by Dr. Lepor. The study, presented at the American Urological Association Annual Meeting and published in the February 2018 issue of Urology, reported on 59 men who underwent radical prostatectomy and met the criteria for FA. Dr. Lepor found that only a small proportion of very low-volume intermediate-risk cancers would have been left untreated if these patients had received FA.
More recently, Dr. Lepor has turned his attention to further defining oncological control following FA, an area of unmet need when it comes to evidence-based counseling for men considering FA. Dr. Lepor and his colleague James S. Wysock, MD, assistant professor in the Department of Urology, acknowledged the lack of data in a comprehensive review published in the June 2018 issue of Reviews in Urology. “More research is needed on whether untreated disease within or beyond the ablation zone will become life-threatening over time,” says Dr. Lepor.
Importance of Follow-Up Care Confirmed by Study
New findings from Dr. Lepor and colleagues represent the first published data on follow-up care beyond one year in the context of FA treatment. The research, published in the June 18 issue of European Urology Oncology, reports on quality of life and disease recurrence in 32 men who underwent prostate-specific antigen (PSA) testing and MRI at 6 months and 2 years following laser FA.
At the two-year mark, MRI reliably identified recurrence of intermediate-risk disease in the ablation zone, investigators reported, providing compelling evidence that patients should undergo interval MRI and biopsy upon positive findings. The procedure had virtually no adverse impact on urinary or sexual function.
It can be challenging to define what constitutes significant or aggressive disease following FA, notes Dr. Lepor. For this study, investigators targeted at least four biopsies in and around the ablation zone and assigned risk based on National Comprehensive Cancer Network guidelines, as follows:
- intermediate risk: Gleason pattern 4
- low risk: Gleason 6 with > 50 percent core involvement
- very low risk: Gleason 6 with < 50 percent core involvement and fewer than 3 positive cores
In the study, eight patients with positive MRIs were found to have cancer in the ablation zone. Of these, six were intermediate-risk, one was low-risk, and one very low-risk. In patients with negative MRI findings, intermediate-risk disease was rarely detected, notes Dr. Lepor.
“The decision to perform biopsy in MRI-negative patients should be guided by whether finding low-risk disease would influence management,” he concludes.
Conclusions Yield New Questions
While more research is needed, it’s clear that ongoing monitoring and testing are essential following FA, says Dr. Lepor.
“Our study provides compelling evidence that many men with a negative biopsy at six months may develop in-field recurrences at two years,” he says. “A positive MRI scan should prompt a biopsy, preferably one that is MRI-guided to the ablation zone.”
The recent follow-up study also highlights the need to refine how FA is performed and how men should be followed, notes Samir Taneja, MD, the James M. Neissa and Janet Riha Neissa Professor of Urologic Oncology; professor in NYU Langone’s Departments of Urology and Radiology and NYU’s Department of Biomedical Engineering; director of urologic oncology; vice chair of the Department of Urology; and genito-urologic program leader at NYU Langone’s Perlmutter Cancer Center.
“The fact that almost 30 percent of men in the study developed intermediate-risk prostate cancer in the ablation zone within 2 years is disconcerting,” Dr. Taneja says. “It suggests that the extent of the ablation zone or delivery of laser energy is inadequate and needs refining. This is consistent with data we have previously published demonstrating that MRI underrepresents the extent and size of many tumors, suggesting that MRI-targeted ablations must incorporate an adequate margin to ensure complete tumor destruction.”
To that end, NYU Langone urologists now employ cryo-ablation and high-intensity focused ultrasound (HIFU) as preferred energy sources to destroy regions of the prostate harboring cancer, because they allow for reliable incorporation of wider margins around the targeted tumor.
Disclosures: Herbert Lepor, MD, is co-owner of MedReviews and has investment interests in Serenity Pharmaceuticals and UroGen Pharma. He previously had an investment interest in SonaCare Medical. Samir S. Taneja, MD, is currently a consultant for Insightec, Sophiris, and Trod Medical, as well as a scientific study investigator for MDxHealth. He also receives book royalties from Elsevier. James S. Wysock, MD, is a paid speaker/consultant for Endocare Inc.; a paid speaker for Fortec Medical, Inc.; a consultant for Boston Scientific; Genomic Health Inc.; Intuitive Surgical Inc.; Precision Biopsy, Inc.; Sonacare, Inc.; Tomer Pharmaceuticals, Inc.; and United Medical Systems.