Dr. Ariane K. Lewis and Dr. Aaron S. Lord review retrospective patient documentation as part of ongoing neurocritical care quality initiatives.
Photo: NYU Langone Staff
With a comprehensive approach to quality improvement, physicians in NYU Langone’s Division of Neurocritical Care bring a renewed focus on outcomes excellence and complication reduction in the most neurologically vulnerable patients.
Applying Research Rigor to Reduce Adverse Events
Several neurocritical care quality initiatives have evolved into NYU Langone–led research projects established to prevent typical hospital-associated adverse events such as pneumonia, urinary tract infections (UTIs), deep vein thrombosis (DVT), and pressure ulcers. Aligned with NYU Langone’s zero harm goal, these research-based initiatives have led to changes in standards of care—and measurable reductions of risk across adverse events.
In the case of Clostridium difficile infection—a leading cause of hospital morbidity—a review of prophylactic antibiotic use following external ventricular drain (EVD) placement found that outcomes improved and C. difficile infection declined when antibiotics were not administered. Similarly, in a review of 58 patients following noninstrumented spinal surgery that was published in 2018 in Neurohospitalist, discontinuation of prophylactic antibiotics was not associated with a significant increase in surgical site infections. “If you look in the literature, EVD infection rates can be anywhere from 5 to 33 percent, and we’ve gone over 18 months without a single infection,” notes Aaron S. Lord, MD, assistant professor in the Departments of Neurology and Neurosurgery and chief of neurology at NYU Langone Hospital—Brooklyn. “This is the result of a multidisciplinary focus on protocols throughout neurology and neurosurgery, and a testament to the quality of our nursing care.”
Similarly, the division has mobilized to prevent central line–associated bloodstream infections (CLABSIs) by identifying high-risk patients and conducting a nursing boot camp to promote CLABSI prevention best practices. Changes in protocol have also helped to reduce ventriculostomy-related infections and catheter-associated UTIs. The new UTI protocol, in which urine is screened for bacteria before culture, has reduced the misdiagnosis of bladder colonization across NYU Langone locations.
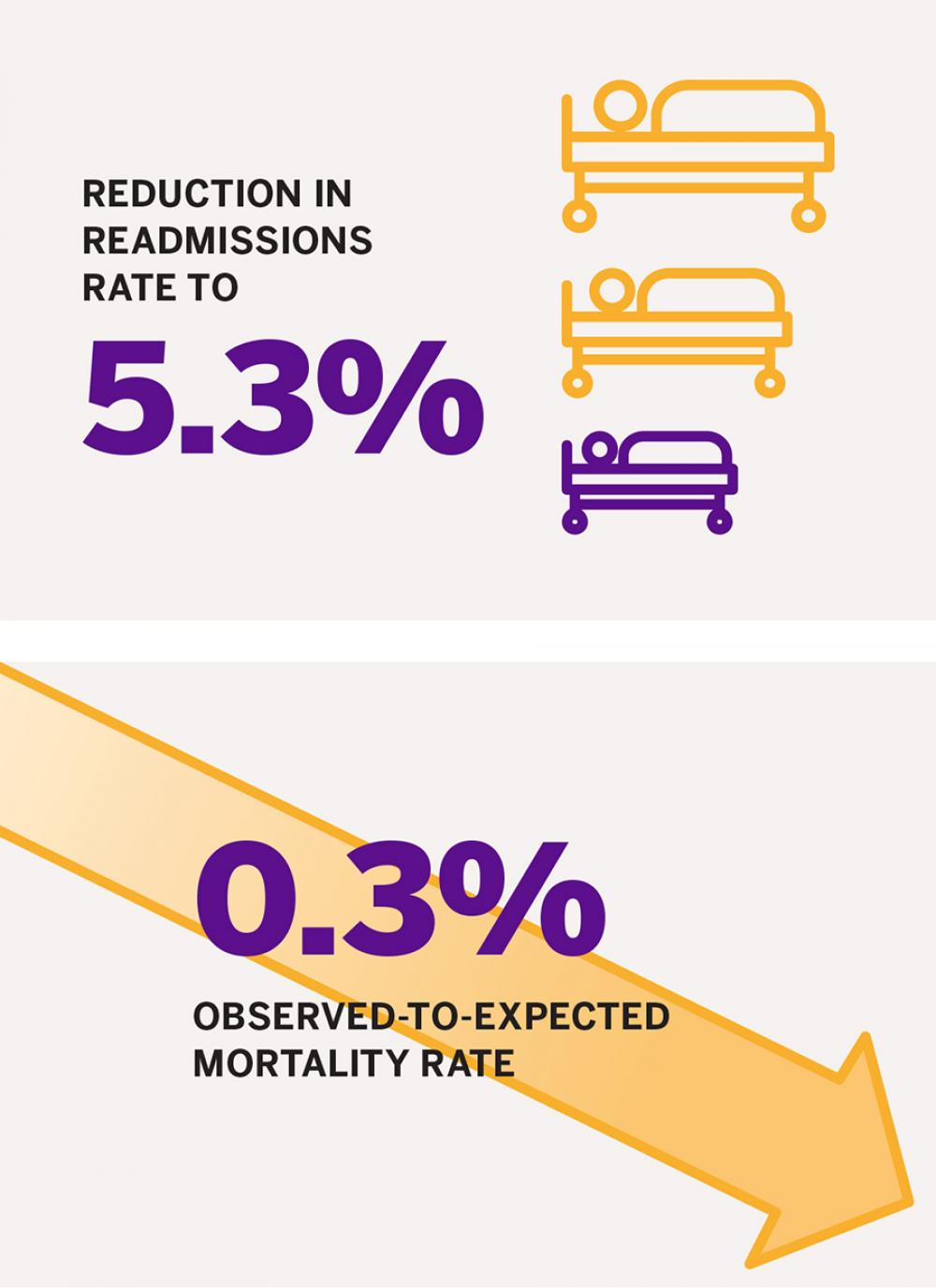
The reduction of these and other adverse events has contributed to improvement in overall hospital quality measures such as readmissions and mortality. The division has reduced its readmissions rate to 5.3 percent, while maintaining a low overall observed-to-expected mortality rate of 0.3 percent against a target of 0.6 percent. “Remarkably, these improvements have been achieved even as the complexity of our patient population, measured by our case mix index, has risen significantly,” notes Dr. Lord.
Aligning Data and Culture to Streamline Care and Drive Change
Several of these neurology-focused quality care initiatives emerged through the institutional adoption of high-reliability organization (HRO) principles. These include weekly HRO rounds in the Neuroscience Intensive Care Unit (NSICU), during which a multidisciplinary care team reviews key quality metrics and safety events. This collaborative, data-driven approach fosters real-time prevention, increases collective accountability, and incubates the development of quality improvement measures across the unit. In the case of patient falls—a common risk for neurocritical patients—HRO rounds have focused on the development of nuanced prevention strategies. Examples include bed alarms, family education concerning safe mobility, and information-sharing concerning fall risk factors.
“HRO rounds focus on transparency of information and accountability across our team—and provide insight into metrics beyond each clinician’s individual patient population,” says Ariane K. Lewis, MD, associate professor of neurology and neurosurgery and director of the Division of Neurocritical Care. “Every week, we’re reviewing the unit’s number of falls and infections, learning from each other’s cases, and, most importantly, discussing prevention strategies as a cohesive team.”
Institution-wide education efforts also include early identification of unexpected stroke symptoms such as sleepiness, and engagement of the stroke team to evaluate such patients on an urgent basis with the goal of preventing more serious strokes.
Alignment of practice patterns with evidence-based protocols has helped standardize care for optimal outcomes across the unit’s core neurological procedures. For instance, when a review of EVD placement revealed some variability—which has been associated with an increased risk of infection—the team’s collective review resulted in the implementation of a standardized dressing across the division’s campuses, subsequently reducing the observed infection rate. “We’ve worked to align practices so that when a patient comes in with a particular neurological condition, that patient’s physicians and nurses all know exactly what the care plan is going to be,” adds Dr. Lewis.
Such alignment demands intentional emphasis on institutional culture focused on streamlining coordination across campuses and ensuring that workflows and tools properly account for those factors that impact quality. Physician documentation, for example, was recently updated to account for a wider range of complications in an increasingly complex patient population. That documentation is shared across all NYU Langone hospitals, as are HRO-promoting resources such as the Departmental Quality Committee, which reviews readmission, mortality, and adverse events data for key metrics and prevention opportunities.
“We are working to have a culture in which residents, nurses, and physicians are all equally focused on quality and speak up when they see something that’s not right,” says Dr. Lord. “That is how we’ve gotten to the point where a patient can expect the same quality neurological care no matter where they present in the NYU Langone network.”
Consistency in the Context of Poor Prognosis
In cases of poor prognosis or end of life, it’s especially important to provide ethical care and appropriate, effective communication with family members, and the division’s policies reflect this approach. Dr. Lewis and her team have conducted a careful review of the institutional protocol around brain death, clarifying the policy in a way that accounts for family or religious objections to neurologic criteria used to declare death. “Management of these objections is variable, and in some cases, it has been highly controversial,” explains Dr. Lewis. “We are one of the few health systems that have taken an in-depth look at this issue and articulated how we handle objections.”
Similarly, a Case Review Escalation Support Team (CREST) was created to support providers in navigating the ethical use of interventions. Dr. Lewis represents neurology as a member of the multidisciplinary team that helps facilitate decision-making about complex cases across the institution. When physicians and a family discuss a question of whether to insert a gastric feeding tube in a patient with severe stroke, for example, the case may be escalated for review by the CREST team.
Across these quality improvement efforts, notes Dr. Lewis, is a desire to recognize the potential for issues and stay ahead of them with an evidence-based strategic plan. “If you’re figuring out how to fix an issue in the moment, it could already be too late,” she says. “When you have an awareness of its potential and are prepared to deal with it, you can deliver care in a way that balances sensitivity and quality medicine.”