Under Dr. Robert Montgomery’s leadership, the NYU Langone Transplant Institute has expanded the viability of donor organs infected with hepatitis C.
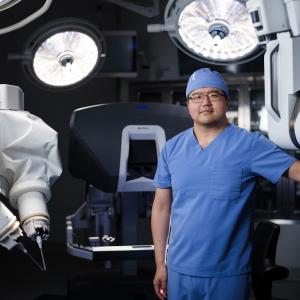
Credit: Brad Trent
For over two decades, Robert Montgomery, MD, PhD, the H. Leon Pachter, MD, Professor of Surgery, has pioneered techniques to make organ transplants more readily available to patients who need them. Among his pioneering innovations are domino kidney transplants—in which multiple living-donor kidneys are swapped so each recipient receives a compatible organ—and the safe use of organs that test positive for hepatitis C. More recently, Dr. Montgomery, director of the NYU Langone Transplant Institute, has championed another potentially transformative approach: using organs from other species, known as xenotransplantation. In 2021, he performed the first investigative transplant of a kidney from a gene-edited pig into a decedent patient whose circulation was sustained artificially. Then, in April 2024, he and colleagues completed the first combined mechanical heart pump and pig kidney transplant surgeries in a living patient. For these breakthroughs, Dr. Montgomery, who is also chair of the Department of Surgery at NYU Grossman School of Medicine, received the prestigious 2024 Jacobson Innovation Award from the American College of Surgeons. We spoke with Dr. Montgomery about these promising advances in transplantation and the next steps in solving the organ shortage.
You inherited a rare form of heart disease and ultimately received a heart transplant six years ago, making you possibly the only transplant surgeon who is also a transplant recipient. From both perspectives, why is the recent progress in xenotransplantation so exciting?
I’m living proof that transplantation works for those who are lucky enough to receive an organ. But I underwent seven cardiac arrests before I was considered sick enough to be prioritized for a heart, and more than 6,000 patients in the United States die each year while awaiting a match. The fundamental problem is that fewer than 1 percent of registered organ donors die in a way that allows for deceased organ donation. We need an additional source for organs, and xenotransplantation is the approach that’s closest to providing one.
During the past two years, we’ve seen successful transplants of pig hearts and kidneys into a handful of living patients, though the organs have ultimately failed or the patients have died from other causes. Meanwhile, experiments on decedents at NYU Langone Health and elsewhere have offered encouraging evidence that pig-to-human transplants can function well over the long term. As someone whose children have inherited my heart disease—meaning they’ll likely need transplants themselves someday—I have lots of reasons to be excited.
So far, xenotransplantation into living patients has been achieved under expanded access authorization from the Food and Drug Administration, which permits experimental therapies for individuals with life-threatening conditions and no other options. Will full-scale clinical trials start anytime soon?
Phase 1 trials are expected to launch in 2025. We’ve already begun the planning process.
What has it taken for xenotransplantation to reach this stage, and what needs to happen before it can start solving the donor organ shortage?
The first step was figuring out the right species to use as the donor. In the 1960s, researchers began experimenting with organs from primates, because they’re very much like us. It wasn’t until the ’90s that we realized pigs were a better choice—in part because they’re less like us and thus less likely to infect humans with any diseases they might carry. Then, we had to develop both gene-editing techniques that would make pig tissue more compatible with the human immune system and immunosuppressant drug regimens that would prevent rejection.
We spent years experimenting with pig-to-primate transplants before transitioning to human decedents. Now that we’ve started working with living humans, we’re realizing there’s a lot we still don’t know. It will likely take another 6 to 10 years to make xenotransplantation viable for widespread use.
What was your goal in the transplant case that combined a mechanical heart pump and a gene-edited pig kidney?
First and foremost, it was about trying to save a life. The patient, Lisa Pisano, a 54-year-old woman with end-stage heart and kidney failure, wasn’t a candidate for a conventional organ transplant because she had several chronic medical conditions. We knew a left ventricular assist device, or LVAD, might prolong and improve her life, but only if she could get a kidney transplant soon afterward. The solution to this catch-22 was a gene-edited pig kidney. A team led by Nader Moazami, MD, chief of heart and lung transplantation and mechanical circulatory support, implanted the LVAD on April 4. We transplanted the kidney eight days later.
The organ functioned well for the first month, enabling us to wean the patient off dialysis and stabilize her cardiovascular function significantly. Unfortunately, she had several episodes of low blood pressure that damaged the kidney, forcing us to remove it after 47 days, and she died six weeks later after her family decided to move her to hospice care. Lisa’s courage and good nature, and her contributions to medicine, surgery, and xenotransplantation, cannot be overstated.
Were there takeaways that could be helpful for other patients?
Absolutely. This was the first time a patient with the device received an organ transplant of any kind. The case showed that LVADs and kidney xenotransplants could eventually be viable for patients with combined heart and kidney failure, and that xenotransplants could become an option for patients who develop kidney failure after a heart pump is implanted.
Your team uses pig kidneys with a single edited gene, versus the multiple edits that some other researchers favor. Why?
One of the advantages of using pigs over other species is that they breed quickly and in large numbers. However, when you add a lot of edits, the animals must be cloned, a slow, laborious process that’s difficult to scale for medical use.
We believe the most important edit involves a gene for a molecule known as alpha-gal that causes a severe immune reaction in humans. By using pigs from herds bred to lack alpha-gal, our team has avoided rejection in every xenotransplant we’ve done so far. If the approach proves sustainable, it will be far easier to meet the needs of patients around the world.
What’s up next in NYU Langone’s xenotransplantation research?
We continue to refine and improve, building on what we know. We’ll take the results from living patients and use them to guide further experiments with our decedent model. Then, we’ll use the results from decedent studies to guide new ones with living patients. I feel very fortunate to be working at an institution with a strong commitment to big-idea research, as well as the resources to support it and the culture of excellence to do so at the highest possible level.