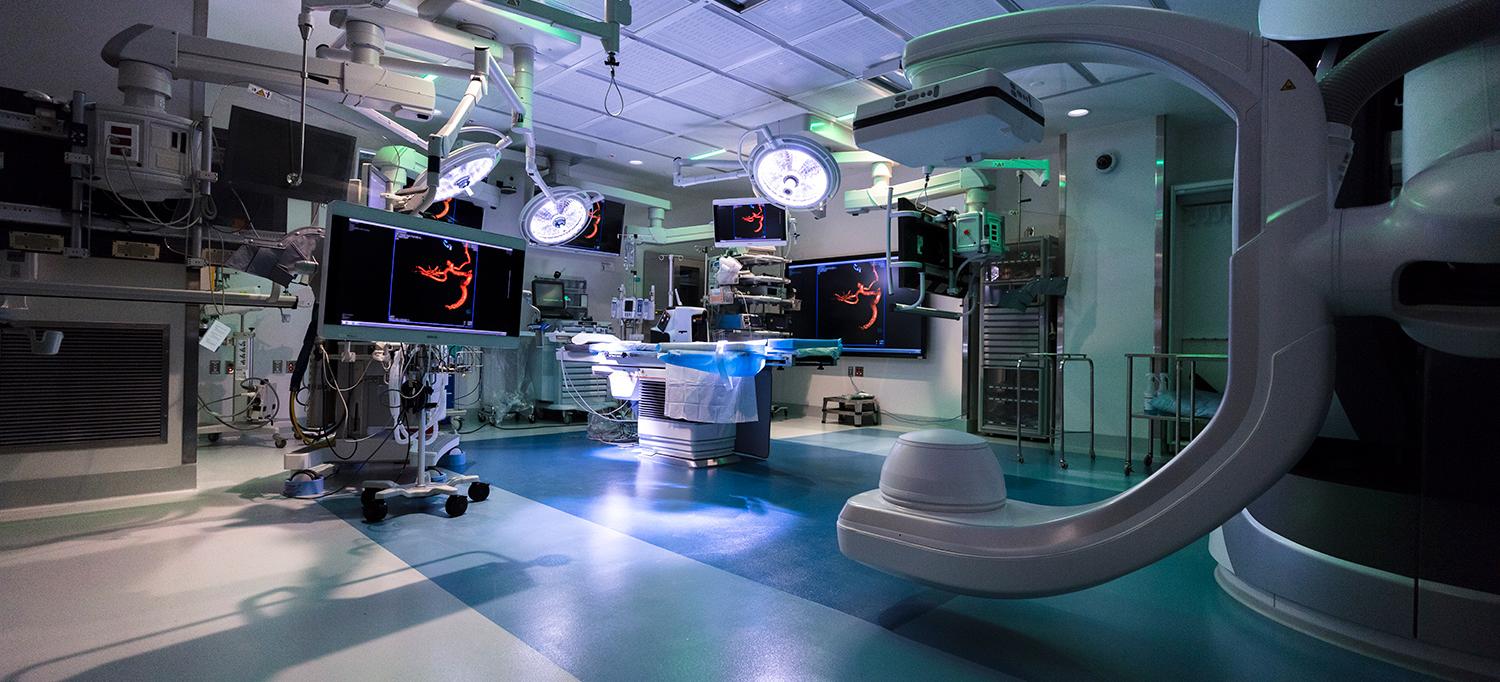
The hybrid operating room is equipped with a state-of-the-art suite of imaging and surgical technology.
Photo: NYU Langone Staff
With a new, dedicated specialty unit that integrates a comprehensive suite of cutting-edge technology, NYU Langone neurosurgeons are poised to set a new standard of care—combining innovation with expertise to foster more precise approaches, unrivaled safety, and expanded treatment options for the most challenging cases.
A Dedicated Neurosurgical Center
Encompassing 2 floors and 7 custom-developed operating room suites within the 830,000-square-foot Kimmel Pavilion, the new space greatly expands the health system’s neurosurgical footprint and solidifies its ongoing investment in technological advancement.
“Two of the rooms are connected to our new intraoperative MRI, two others are shielded for intraoperative CT, and we have a dedicated neurovascular surgery room with robotic three-dimensional angiogram imaging capabilities,” says John G. Golfinos, MD, associate professor of neurosurgery and otolaryngology and chair of the Department of Neurosurgery. “The combined potential of these tools lays the groundwork for new milestones to be set in patient care and outcomes.”
The neurosurgical team functions as a single closed-loop system of specialized expertise, able to discern complications quickly and mobilize readily with needed interventions. “And on top of this collective insight, our patients are surrounded by next-generation technology that continues to evolve and transform how we approach neurosurgical care,” adds Dr. Golfinos.
Intraoperative MRI Delivers Unprecedented Surgical Precision
The new intraoperative MRI provides neurosurgeons with real-time, high-resolution imagery that guides their approaches and circumvents neurosurgical challenges, enabling a level of precision that decreases complications and confirms total tumor resection.
NYU Langone is one of the few health systems in the nation that utilizes a fixed-magnet setup and 3-Tesla high-resolution technology, a combination that results in unsurpassed functional views of both anatomy and pathology.
An integral presurgical and intraoperative collaboration with neuroradiologists provides both advance guidance and real-time refinement. “Based on the patient’s prior MRI study, the neuroradiologist predetermines sequences to be done when the patient comes into the intraoperative MRI suite,” notes Girish M. Fatterpekar, MD, associate professor of radiology and chief of neuroradiology. “Time is of the essence during surgery—so this advance planning allows us to perform as few sequences as possible, harnessing the key information needed to determine the best approach.”
Deeper intraoperative insight is transforming the neurosurgical team’s treatment of complex tumors, allowing them to achieve full resection by distinguishing margins from normal brain tissue, identify complications such as hemorrhage with a new level of accuracy, and circumvent problems such as shifting brain tissue that typically obscures tumor margins and is missed by less precise intraoperative MRI. “Intraoperative MRI availability makes surgery more efficient and safer for our patients and allows us to proceed confidently with resections, armed with insight we never had before,” says Dr. Golfinos.
Together, Technology Enhances Outcomes
Close collaboration among key stakeholders during the planning process enables neurosurgeons to play a critical role in evaluating evidence-based technologies and determining the optimal combination of innovations to invest in, with an eye toward better outcomes. The result is an infrastructure of future-ready technologies that are taking neurosurgery to new levels of intricacy.
One such technology, advanced PET MRI, utilizes an on-campus cyclotron to produce radioactive tracers that enhance the visualization of specific tumor types.
“Conventional imaging can identify the lesion but has difficulty identifying the tumor type,” notes Dr. Fatterpekar. “The radiopharmaceutical tracer complements the conventional MRI by pinpointing the tumor type and mapping its extent, and it can detect other ‘silent’ tumors of the same type elsewhere in the body. It also plays an important role in distinguishing tumor recurrence from treatment-induced changes, a limitation of conventional imaging.”
A dedicated spinal navigation room in the new neurosurgical suite brings advanced, real-time spinal navigation to the operating table. The new setup enables imaging-enhanced approaches once limited by pre- and postoperative imaging alone. “With the integration of advanced spinal navigation, we’re working toward navigated functional spine surgery, which is a first,” says Anthony K. Frempong-Boadu, MD, associate professor of neurosurgery and director of the Division of Spinal Surgery.
A single-plane digital fluoroscopy machine that uses novel perfusion software enables simultaneous open surgery and interventional procedures, while 4-D angiography visualizes blood flow through vascular malformations in the brain for enhanced navigation while treating lesions.
Consolidating the technologies is Brainlab Buzz, a customized multimedia platform that puts all available information at the care team’s fingertips—an innovation in clinical informatics that amplifies the benefits of individual procedural technologies.
“We’ve amassed a truly unparalleled collection of all the leading neurosurgical technologies in one place,” notes Dr. Golfinos. “Walking into these operating rooms, you know you’re looking at the future of neurosurgery. We are at the forefront of precise, minimally invasive, imaging-driven advances, the possibilities of which we are just beginning to unearth with these resources.”