System-Wide Emphasis on Quality Fuels Necessary Innovation in Patient Care

Emphasizing collaboration and innovation, ENT specialists joined the multidisciplinary COVID-19 care teams comprising physicians and staff, including nurse clinicians like Michael Abejo, across NYU Langone Health who worked tirelessly to manage the influx of patients with COVID-19.
Photo: Jonathan Kozowyk
As the coronavirus disease (COVID-19) pandemic took hold in New York City—demanding both a quick and a coordinated response—care teams across NYU Langone Health were redeployed across the system’s hospital network to support critical patient care. Within the Department of Otolaryngology—Head and Neck Surgery, a significant number of physicians and nurses were rapidly assigned to COVID-19 intensive care units (ICUs) and converted medical floors, while other team members remained focused on safely providing emergent otolaryngology care and surgery. As the dynamic situation evolved, each day shedding more light on the novel virus, the team continued to emphasize quality and multidisciplinary collaboration to support the health system in not only meeting the needs of critically ill patients, but also innovating to mitigate the pandemic’s most dangerous risks.
Maintaining Quality Through Crisis
As a massive influx of patients with COVID-19 began to inundate hospitals across New York City, an unprecedented challenge emerged: how to provide high-quality care while treating an idiosyncratic virus that posed more questions than medicine could immediately answer.
“Now we have so much guidance, based on patient data and emerging best practices, to help our physician colleagues worldwide respond to the virus and protect themselves,” notes J. Thomas Roland Jr., MD, the Mendik Foundation Professor of Otolaryngology, professor in the Department of Neurosurgery, and chair of the Department of Otolaryngology—Head and Neck Surgery. “But initially we knew very little about the disease, so it was like a live, real-time case example of leadership requiring coordination across administration, research, clinical care, and continued education of residents and fellows.”
The department’s emphasis was twofold: overcoming fear so doctors felt comfortable treating patients, and creating an effective communication flow up and down the chain of command. New protocols, such as a daily newsletter tracking case data and best practices—including the proper ways to don and doff personal protective equipment (PPE)—became critical to the management of patients with COVID-19, which numbered 21,000 suspected infections, 6,000 admissions, and 1,200 ICU admissions from March 14 to June 2 at NYU Langone alone. From residents treating patients to department leaders managing response strategy, observations and innovations were shared rapidly and implemented system-wide, fueling NYU Langone’s strong COVID-19 survival data. Rapid-response communication techniques also served to protect COVID-19 caregivers, the vast majority of whom were spared exposure to the infection via patient care.
“These lessons learned through the pandemic offer a road map for better, safer patient management moving forward, and many innovative technologies and procedures evolved that will likely continue after the COVID-19 crisis abates.”—J. Thomas Roland Jr., MD
A strong communication chain, and the intelligent decision-making it supports, has enabled the multidisciplinary COVID-19 care teams to think about patient care beyond short-term survival. “We’ve approached these cases from a long-term vantage—not just treating the acute presentation of the disease, but thinking down the road about patients’ quality of life as they recover from both COVID-19 and the treatments we provide,” explains Dr. Roland. “And that means innovating as we go.”
Rethinking Tracheostomy as Treatment
One such innovation was a project initiating early tracheostomy in patients at day 5 of the disease’s course, as opposed to the 21-day mark suggested in established guidelines. The project was conceived by Luis F. Angel, MD, professor in the Departments of Medicine and Cardiothoracic Surgery, who had adopted percutaneous tracheostomy to facilitate faster recovery in patients with lung transplant. Faculty, residents, and fellows from otolaryngology—head and neck surgery, pulmonary medicine, and thoracic surgery collaborated to prevent poor outcomes observed in intubated patients—who had death rates as high as 80 percent—by offering patients percutaneous or open tracheostomy at day 5. “This was a shift in conventional wisdom, which left tracheostomy as a last resort for dying patients requiring transport to hospice or chronic care facilities,” notes Dr. Roland.
The early intervention became an effective treatment approach enabling patients to mobilize, free of the sedation-induced paralysis associated with ventilation. A tracheostomy care team was formed to triage side effects of the procedure, and team members were often called in overnight to treat site bleeding or associated bleeding from the oral cavity or nose.
The benefits of the procedure quickly proved to far outweigh any risks; the movement and pulmonary toileting—methods to clear airways of mucus—facilitated by tracheostomy in more than 250 patients observed at NYU Langone resulted in a survival rate of 90 percent, far greater than the estimated rate of 20 to 50 percent in critically ill patients.
The approach also yields long-term benefits for these patients. “If a patient is intubated for three weeks, there’s a significant risk for laryngeal stenosis and scarring, vocal cord paralysis, and subglottic stenosis,” notes Dr. Roland. “With a tracheostomy, those risks are avoided, which means better long-term outcomes for our patients recovering from this disease.”
Surgical Innovation Worth Sustaining
Necessary COVID-19 innovation also emerged in the operating room, where surgeons continued to address cases meeting emergent criteria during the height of the pandemic, and subsequently when elective surgeries commenced in May. PPE protocols were examined, particularly in the context of procedures that tend to cause aerosolized fluids to permeate the operating room. Research informed new protocols, including novel, three-dimensional (3D)–printed face shields developed by medical students. Special draping techniques covering most of the surgical site but allowing access, developed by department fellows, enabled the continued use of intraoperative microscopes without the release of aerosolized fluids.
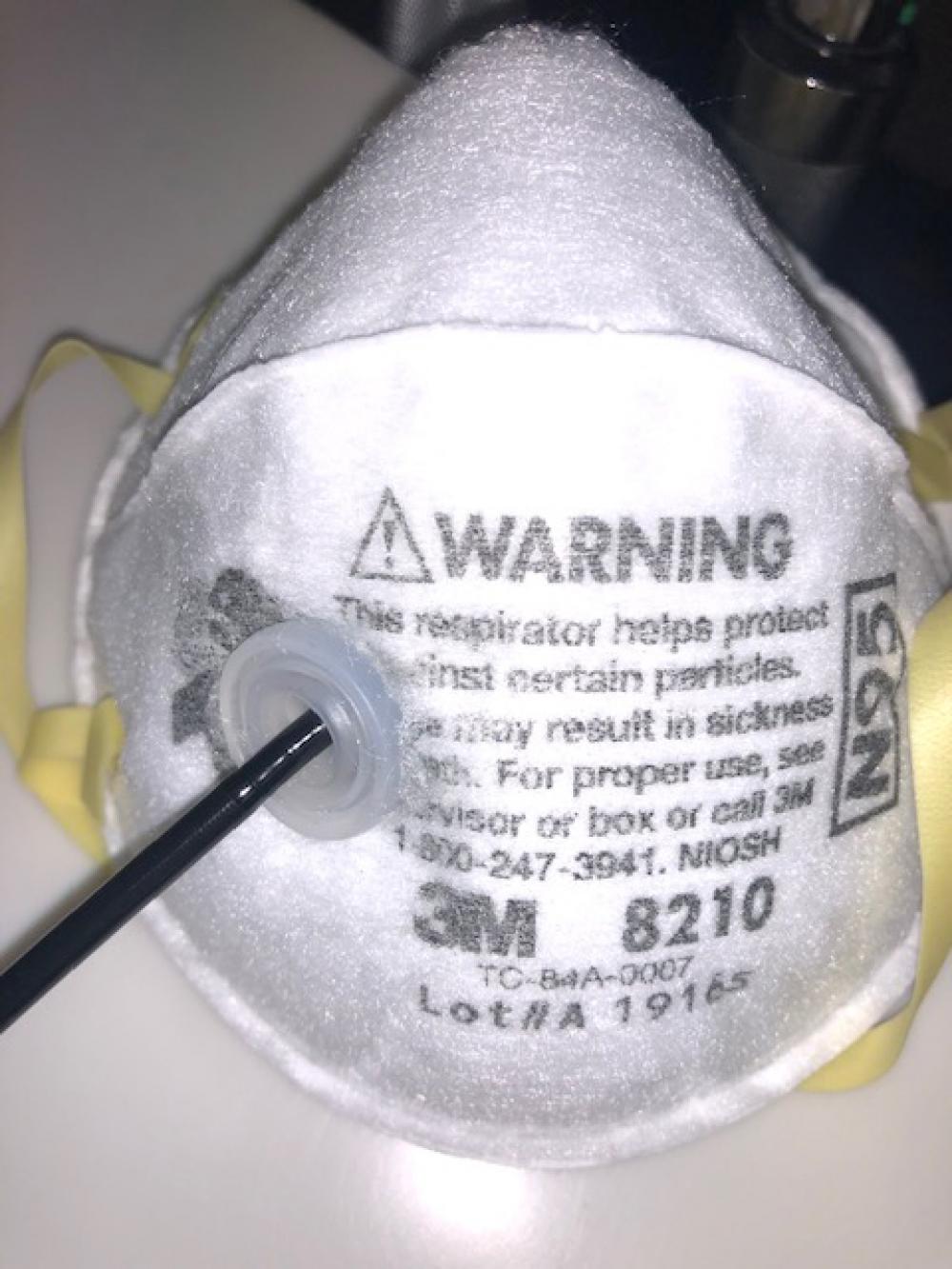
Erich P. Voigt, MD, director of the Division of General Otolaryngology and Sleep Surgery, developed a patent-pending N95 mask that has a one-way valve for safe nasopharyngoscopy evaluations. The procedure is considered a potential “super-spreader” event for its typical high release of fluids when a tube is introduced into a patient’s nasal cavity, making innovation necessary to enable its safe delivery as a standard of patient care, through and beyond the pandemic’s peak.
Similarly, as emergency otolaryngology patient care and surgery were sustained through the worst of the pandemic, safety demanded elevated sterilization and testing protocols including on-the-spot PCR testing, appropriately pressurized rooms, and PPE. These and other patient management protocols have continued as the delivery of elective, non-emergent procedures was reinstated on the basis of priority categorization of different diagnoses.
“Though otolaryngology is not on the front lines of COVID-19 research like other specialties such as immunology, our specialty puts us at very high risk due to close contact around our patients’ faces,” notes Dr. Roland. “These lessons learned through the pandemic offer a road map for better, safer patient management moving forward, and many innovative technologies and procedures evolved that will likely continue after the COVID-19 crisis abates.”
Collaboration Yields Collective Progress
The medical system’s shared reliance on continued quality improvement and multidisciplinary collaboration was tested and proved by the pandemic, as interdisciplinary teams worked together to stem the physical and emotional impacts of the novel virus.
“These months have underscored the vitality of our shared resources and workflows—that you can achieve better patient care, even through crisis, working together,” adds Dr. Roland. “As each day spurred new information based on collective discoveries, unnecessary fear and anxiety were mitigated with elevated precautions, frequent communication, and intelligent decision-making based on observation and analysis—fine-tuning our ability to innovate and expanding our collective emotional strength.”