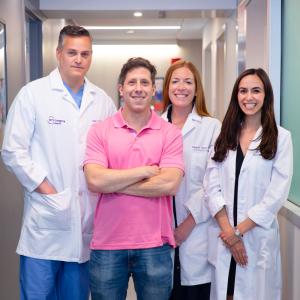
Phil Passen shows off the scar from the complex aortic surgery performed by Dr. Mark Peterson. Accompanying them are Meghan Taylor, NP, MSN, and Jodi Feinberg, NP, MSN, assistant program director for cardiothoracic surgery.
Credit: Haley Ricciardi
Phil Passen had no reason to suspect he was anything less than superbly healthy. At 46, he ran 30 miles a week, boxed recreationally at his local gym, and relished his fast-paced job in finance. During his annual physical at NYU Langone Health in 2016, however, his primary care physician, Anelise M. Engel, MD, detected a slight heart murmur. She referred Passen to cardiologist Olivier Frankenberger, MD, PhD, who ordered an ultrasound. The resulting images revealed a congenital heart defect known as a bicuspid aortic valve.
A normal aortic valve has three flaps, or cusps, that open and close with each heartbeat; a bicuspid valve, which occurs in only 1 to 2 percent of the population, has only two. Over time, valves with only two cusps are more prone to calcify, narrowing the valve and restricting blood flow, a condition called aortic stenosis. “Dr. Frankenberger told my wife, Priscilla, and me that most patients eventually need to have the valve replaced,” Passen recalls. “At that point, though, my stenosis was mild, so he advised that we watch and wait.”
Passen had regular checkups until he moved to Miami in 2019. Soon after, the COVID-19 pandemic hit, making it impossible to schedule an appointment with a new cardiologist. Because he remained free of the telltale symptoms, such as shortness of breath or lightheadedness, Passen then put off seeing a doctor for another three years. When he finally did, in May 2023, he got the news he’d long dreaded: he needed surgery.
Passen was offered two options. He could choose a mechanical valve, which would require him to be on lifelong blood thinners and force him to abandon his athletic pursuits, or a cow valve, which would potentially require replacement every 10 to 15 years, a daunting prospect given his relative youth. “Both alternatives scared me,” Passen says.
Passen quickly flew to New York. After running several tests, Dr. Frankenberger confirmed that a new valve was needed, though it could safely wait a few months. Then, he referred Passen to Mark D. Peterson, MD, PhD, an internationally recognized leader in rebuilding dysfunctional aortas and aortic valves. Dr. Peterson, who had recently joined NYU Langone Heart as system director of aortic surgery, told Passen about a third option, a complex and demanding surgery known as a Ross procedure. The technique requires placing the patient on a heart–lung bypass machine, replacing the defective aortic valve with the patient’s own pulmonary valve—a kind of self-transplant—and then replacing the pulmonary valve with one from a deceased donor.
The open surgery is more complex than a conventional aortic valve replacement, but with a substantial payoff. “When performed by a skilled surgeon and for the right patient, the Ross procedure offers a unique opportunity to restore health, longevity, and quality of life,” says Dr. Peterson. “It provides decades-long durability while eliminating the need for blood thinners.”
The challenge is finding a qualified surgeon. Few specialists possess the necessary expertise and skill, but Dr. Peterson is a senior member of that elite corps. He has performed many hundreds of reconstructive aortic root procedures, including the Ross procedure, during the past 15 years and does several each week alongside other intricate surgeries, including challenging aortic aneurysm repairs. Dr. Peterson’s track record and NYU Langone’s No. 2 ranking for cardiology and heart surgery in U.S. News & World Report’s Best Hospital rankings persuaded Passen to take the leap.
The four-hour surgery took place on March 26, 2024. It went smoothly, and Passen’s recovery benefited from NYU Langone’s groundbreaking fast-track protocol after cardiac surgery. “Put simply, we get patients up and moving as soon as possible,” says Jodi Feinberg, NP, MSN, assistant program director for cardiothoracic surgery. Studies show such measures lead to fewer postoperative complications, faster recovery, and shorter hospital stays. Within two hours, Passen was walking laps around the intensive care unit. He was discharged after just three days, well below the average for a Ross procedure. (It’s also consistent with NYU Langone’s system-wide quality control measures, which ensure surgical patients go home earlier here than at 95 percent of comprehensive academic medical centers, as rated by Vizient Inc., a leading healthcare performance improvement organization.)
Passen flew back to Miami two weeks later. In a little over a month, he was back to running and boxing. Now 54, he’s grateful to Priscilla and his daughter, Sofia, age 9, for their support throughout his medical ordeal—and to NYU Langone clinicians for restoring him to robust health.
“Physically, I feel better than ever, and it’s a huge relief to be free of the worry I carried for years that something might happen to my heart,” says Passen, who returns periodically for follow-up visits with Dr. Peterson and Dr. Frankenberger. “My future would have looked very different if I hadn’t had the opportunity to choose this procedure, and if not for the attentiveness, care, and expertise of everyone on my team.”