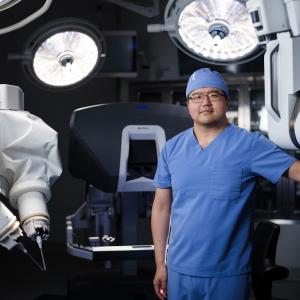
Dr. Lee C. Zhao
Photo: NYU Langone Staff
Urologists at NYU Langone lead the field in expertise in the use of robot assistance during laparoscopic repair of ureteral strictures. Lee C. Zhao, MD, first described the technique of robotic ureteroplasty with buccal mucosal graft for management of a proximal ureteral stricture in the September 2015 issue of Urology. Dr. Zhao is assistant professor in the Department of Urology, director of male reconstructive surgery, and co-director of transgender reconstructive surgery in Transgender Surgery Services.
A Proximal Ureteral Stricture Failed to Resolve
In a current case, a 40-year-old male patient was referred to NYU Langone after undergoing multiple procedures that failed to resolve a 4-cm proximal ureteral stricture that had developed as a result of treatment with ureteroscopy and laser lithotripsy for an impacted ureteral stone.
Before seeking treatment at NYU Langone, the patient underwent ureteral dilation, endoureterotomy, and placement of a stent. After stent removal, he developed pain and hydronephrosis, necessitating nephrostomy placement at the outside institution. Using robot-assisted laparoscopy, NYU Langone urologists successfully achieved ureteral reconstruction with a buccal mucosa onlay graft.
Location and Extent of Stricture Guide Surgical Management
“At NYU Langone, we typically perform ureteroneocystostomy in patients who have distal ureteral strictures,” explains Dr. Zhao. “If the patient has a mid-ureteral stricture with sufficient bladder capacity, a Boari flap can be utilized. In patients with proximal ureteral strictures where a direct connection from the ureter to the renal pelvis is possible, pyeloplasty is performed,” he continues.
“Onlay of buccal mucosa or an appendix flap can be used for ureteral reconstruction in large proximal strictures. If a long segment of the ureter is missing, ileal ureter transposition is a potential option, but potential bowel complications include ileus and metabolic acidosis,” Dr. Zhao says. “Autotransplantation may provide a solution as a last resort, although it is associated with the risk of vascular injury to the recipient vessels.”
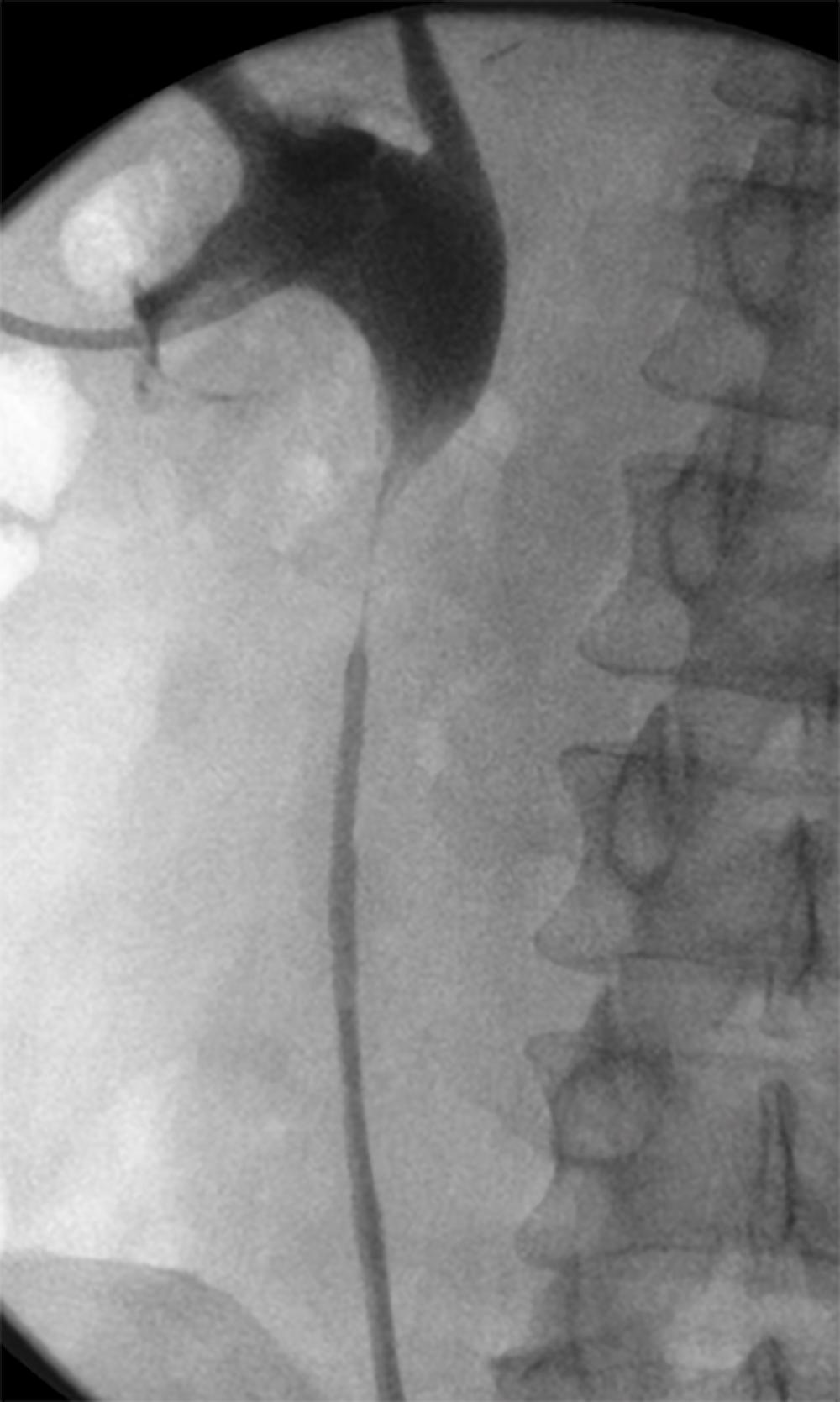
Preoperative anatomic assessment of the stricture includes evaluation of the degree of obstruction, relative renal function, and surrounding vascular anatomy. In this case, antegrade and retrograde pyelograms were performed to delineate the patient’s 4-cm proximal stricture (Figure 1).
“A stent may obscure the delineation between the normal ureteral segment and the stricture,” Dr. Zhao explains, “so we remove the ureteral stent before reconstruction, to allow the stricture to mature. If the patient is dependent upon a ureteral stent, we place a nephrostomy tube before stent removal.”
Intraoperative Identification of Diseased Tissue Is Critical to Success
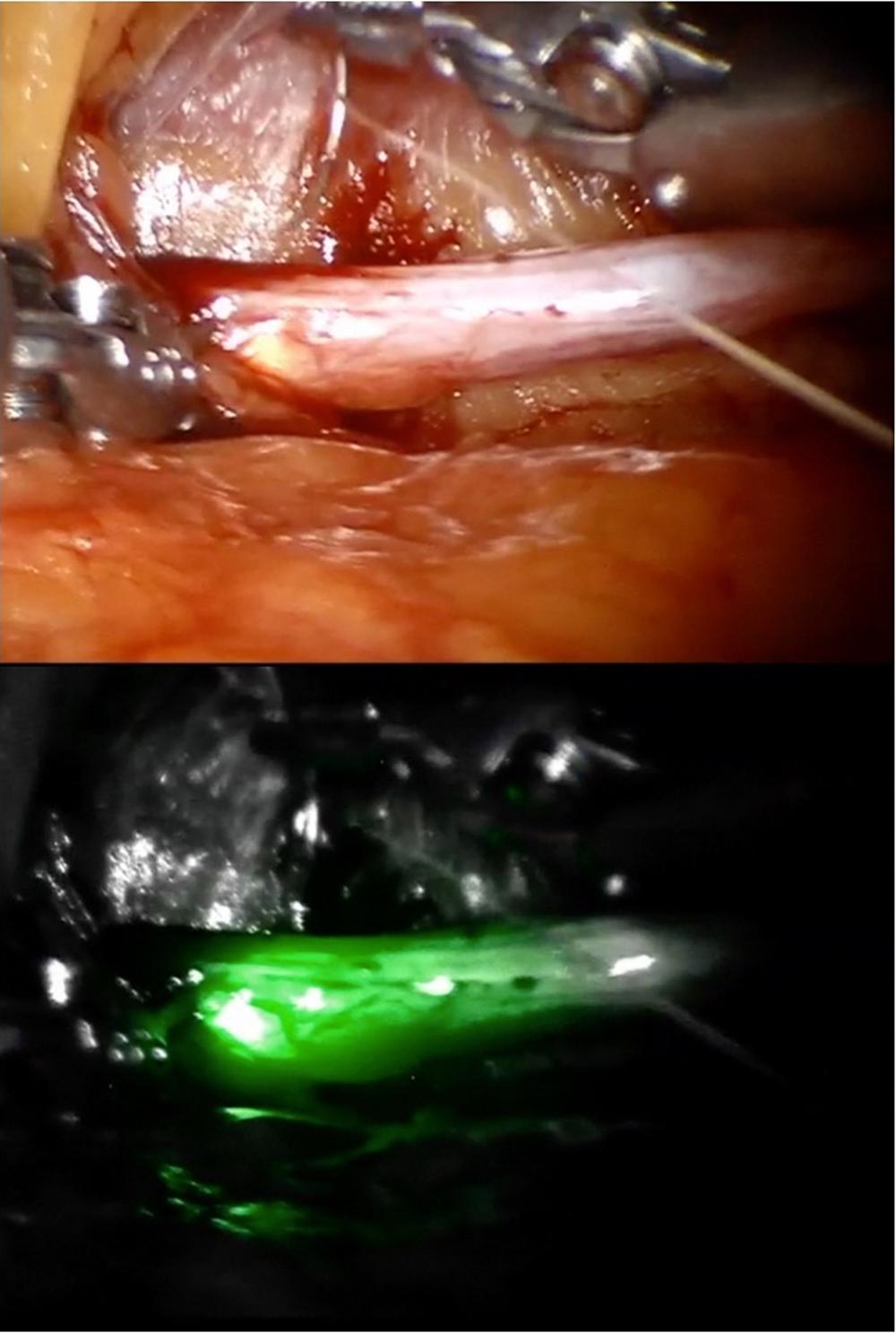
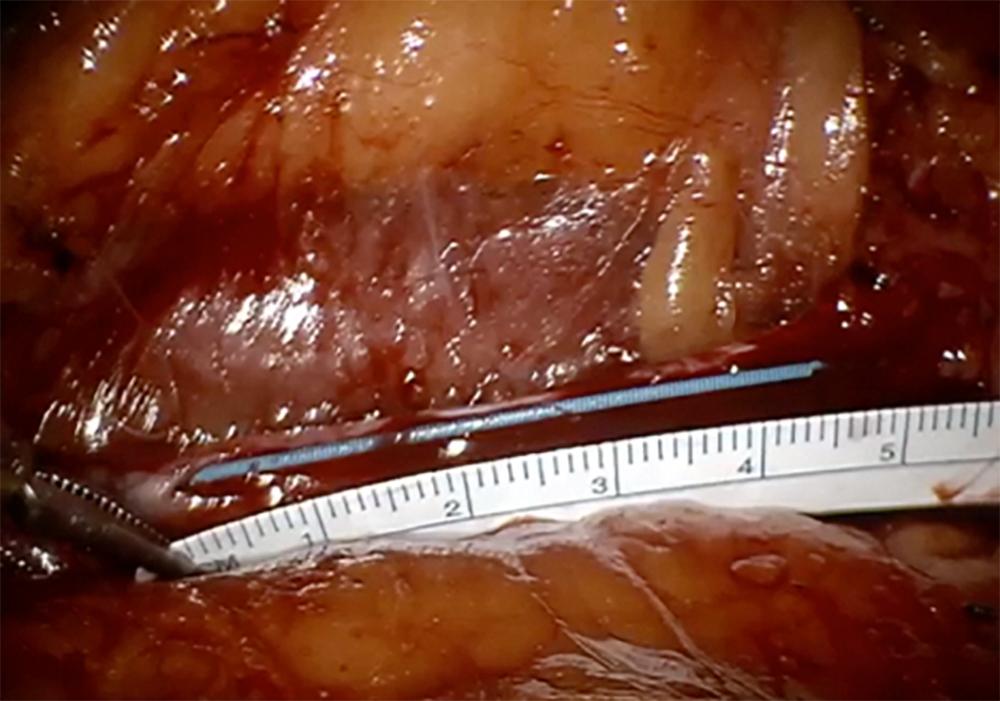
After transport to the operating room, the patient was placed in the flank position with the ureter exposed. Four robotic trocars were placed. Intraoperative ureteroscopy with FireFly® fluorescence imaging was performed to identify the location of the stricture (Figure 2). An incision was performed on the anterior surface of the narrowed segment of the ureter until a 4-cm opening was achieved. (Figure 3).
Buccal Mucosa Tissue Characteristics Are Ideal for Urinary Tract Reconstruction
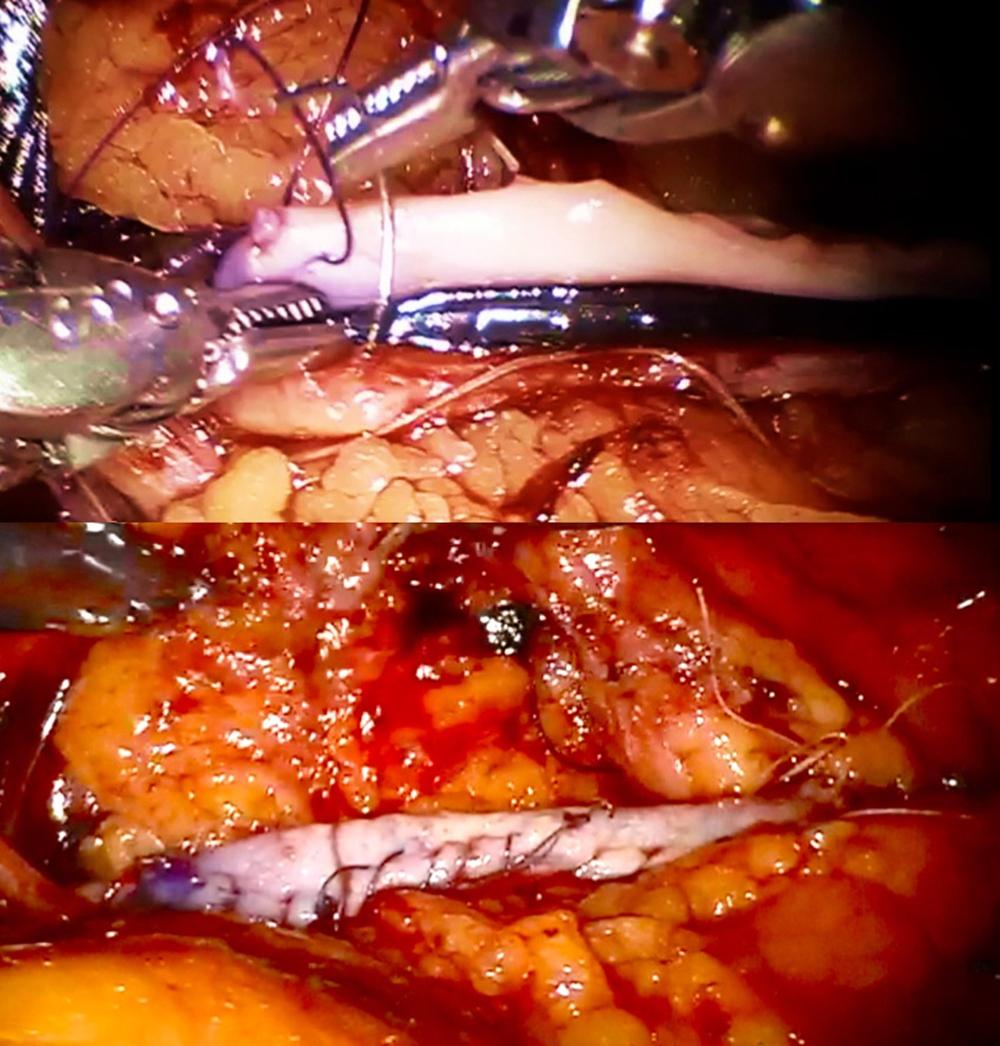
After measurement of the defect, a buccal mucosa graft of appropriate size was harvested from the cheek and passed into the abdomen. Buccal mucosa has a thick epithelium, and the lamina propria is highly vascularized, making it a good choice for repair of ureteral strictures.
The graft was sutured on as an onlay until the ureteral defect was covered entirely (Figure 4). An omental flap, which had been mobilized during the initial dissection, was then secured around the anastomosis at the psoas muscle and sutured to the graft to provide vascularity.
A Promising Alternative Treatment Option with a Successful Outcome
The patient was discharged on postoperative day one, and the ureteral stent was removed after four weeks. The patient had complete resolution of flank pain. Subsequent renal ultrasound showed no hydronephrosis, and renal scan demonstrated good drainage. This case and other case reports and series demonstrate the expansion of treatment options and improved patient outcomes achieved through the use of laparoscopy with robotic assistance in the performance of challenging urologic surgeries.