Dr. Howard Riina combines surgical expertise with access to advanced technology, enabling him to tackle complex surgical cases.
Photo: Keiji Drysdale
When imaging prompted by recurrent neurological symptoms revealed a cavernous malformation in the brain, a 49-year-old patient was referred to experts at NYU Langone’s Center for Stroke and Neurovascular Diseases for surgical intervention.
There, a carefully planned multidisciplinary approach guided by advanced technology enabled a successful resection and restored the patient’s quality of life.
A Hemorrhage at the Brain’s Epicenter
A presentation of headaches, visual problems, and hemisensory loss at another institution precipitated the diagnosis of obstructive hydrocephalus and intracranial hemorrhage. Imaging subsequently revealed a cavernous malformation at the tectum, and active surveillance was recommended.
Two years later, imaging prompted by recurring symptoms revealed a repeat hemorrhage at the posterior tectum, and studies four months later showed expansion of the cavernous malformation without resorption of the hemorrhage.
Functional Decline, Hemorrhage Risk Compel Treatment
The patient’s increasing sensory abnormalities and headaches led Howard A. Riina, MD, professor of neurosurgery, neurology, and radiology, vice chair of the Department of Neurosurgery, and director of the Center for Stroke and Neurovascular Diseases, to consider surgical intervention, a challenging option that had been ruled out by other experienced surgeons.
The patient’s history also supported surgery: While there is a 0.25 percent to 2.3 percent initial hemorrhage rate, it climbs to between 30 percent and 40 percent for patients with symptomatic recurrent hemorrhage, making the need for resection more urgent.
In light of the technical challenges and significant risks, Dr. Riina’s extensive surgical experience coupled with advanced imaging would be critical to the successful management of this case.
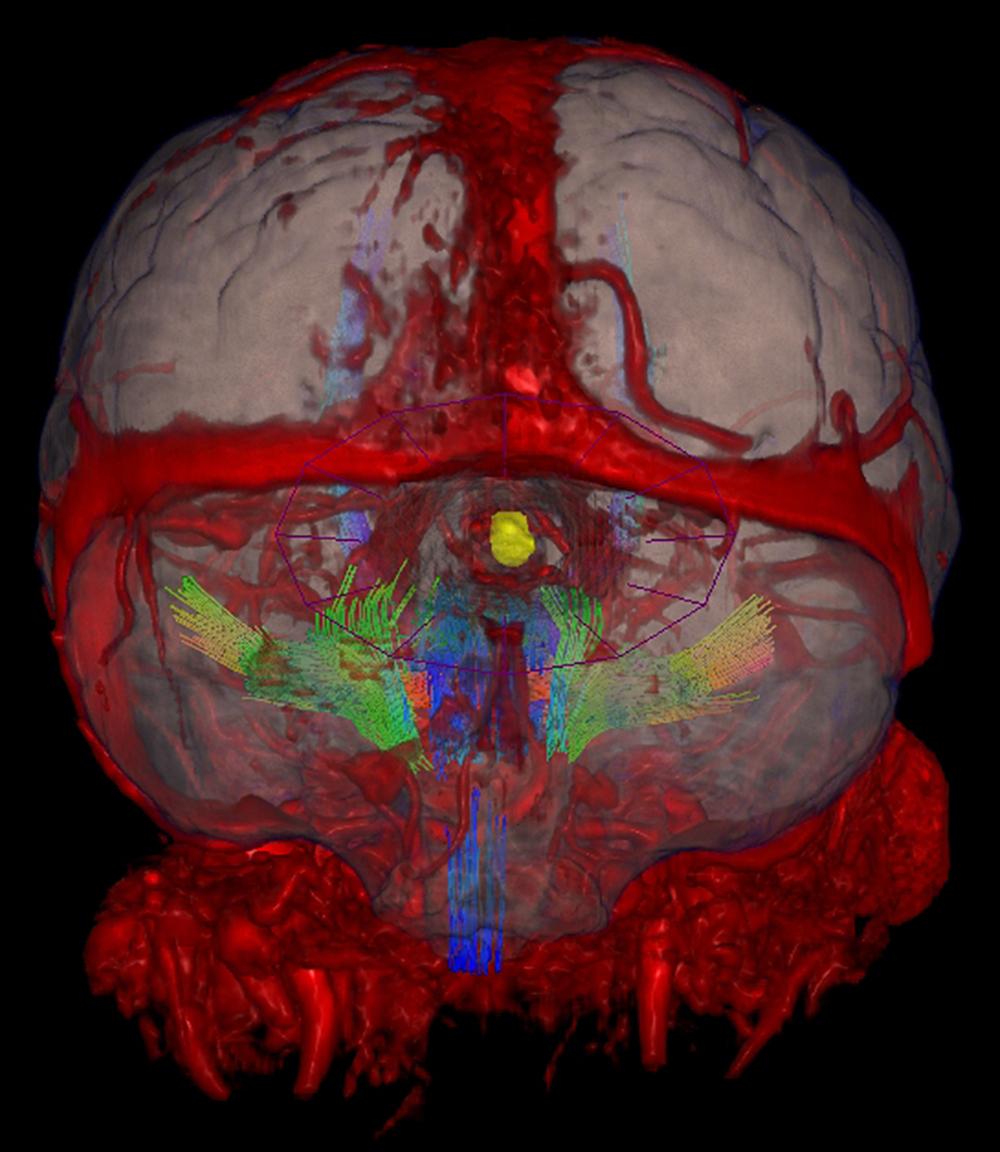
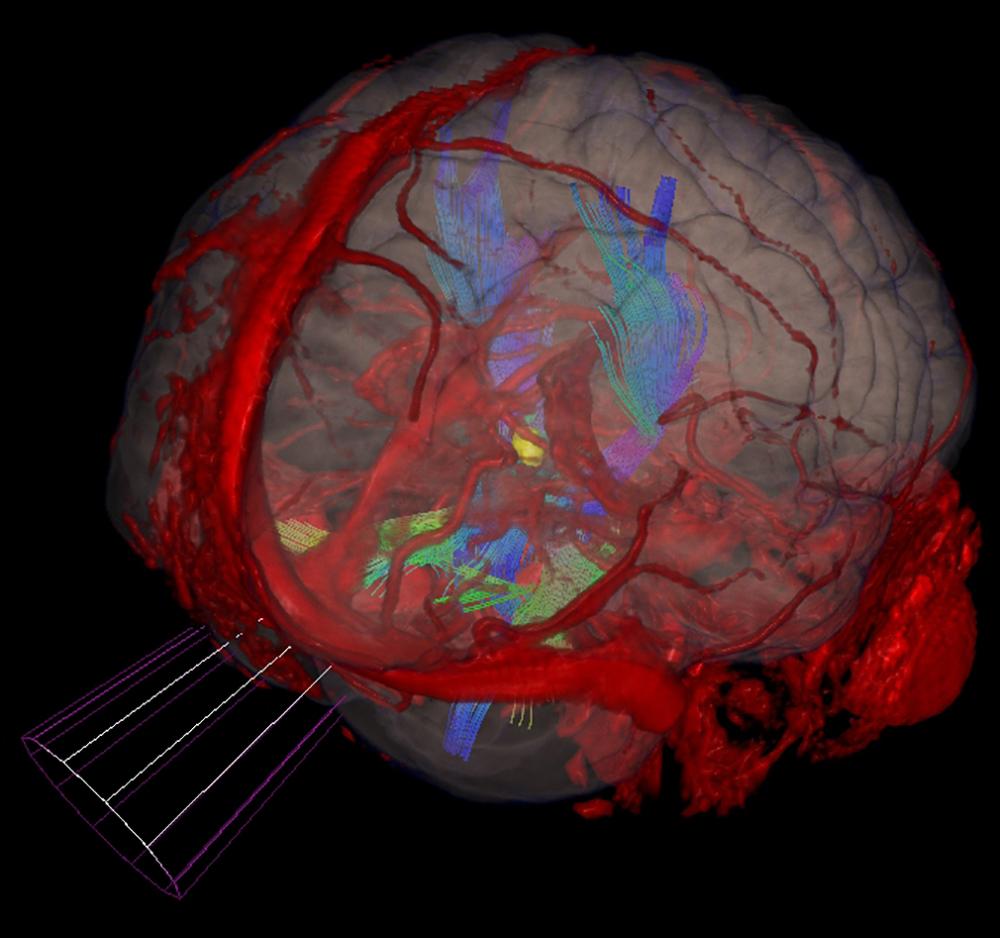
“Our imaging capabilities are critical in a case as complex as this one,” says Dr. Riina. “Superimposing a fused image of the brain and vascular anatomy on the patient both guides our approach and allows us to avoid all critical vascular structures and motor pathways so we can confidently achieve full resection.”
Advanced Imaging Plots a Path for Resection
A multi-planar, multi-sequential MRI showed a slightly smaller malformation with a hemosiderin rim measuring 1.2 cm x 1.1 cm in the right paramedian tectum, with associated evidence of chronic hemorrhage.
A developmental venous anomaly inferior to the lesion drained into the right ambient cistern, and a ventriculoperitoneal shunt catheter was identified with a right frontal approach and termination in the region of the third ventricle.
Guided by the imaging results, Dr. Riina determined that a subtentorial supracerebellar approach would enable access for complete resection while avoiding damage to critical structures. Image overlays by diffusion tractography of the corticospinal tract provided enhanced analysis of two-dimensional images to elucidate the approach.
“We chose to operate with the patient in the sitting position to drop the cerebellum from the field by gravity, providing greater exposure while avoiding traction on the cerebellum,” says Dr. Riina.
With a comprehensive plan in place, Dr. Riina began the operation by identifying the transverse sinus, then carried a midline incision to the bone, extending into the suboccipital region, avoiding exposure of the C1 arch. The inferior half of the transverse sinus was exposed by suboccipital craniotomy, and the dura was opened to expose the supracerebellar region.
The trajectory to the right superior colliculus was confirmed before two bridging veins were coagulated and incised, further relaxing the cerebellum to facilitate the approach to the pineal recess. Under direct visualization, the arachnoid was opened and the hematoma gradually came to the surface, accompanied by a portion of the cavernous malformation.
Entrance into the cavity resulted in evacuation of the hematoma, and the cavernous malformation was removed using micro tumor biopsy forceps. Visual inspection confirmed no residual malformation remained.
Optimizing Outcomes in the Context of Complexity
In this case, a combination of unparalleled expertise and advanced imaging enabled Dr. Riina to provide surgical treatment that few medical teams would have been equipped to perform.
“This case required a unique combination of advanced imaging and a highly refined approach that together enabled the planning and execution of a successful resection,” he notes. “With these capabilities, we reduced a typical eight-hour operation down to three and sent this patient home safely two days later with a complete resolution of symptoms.”