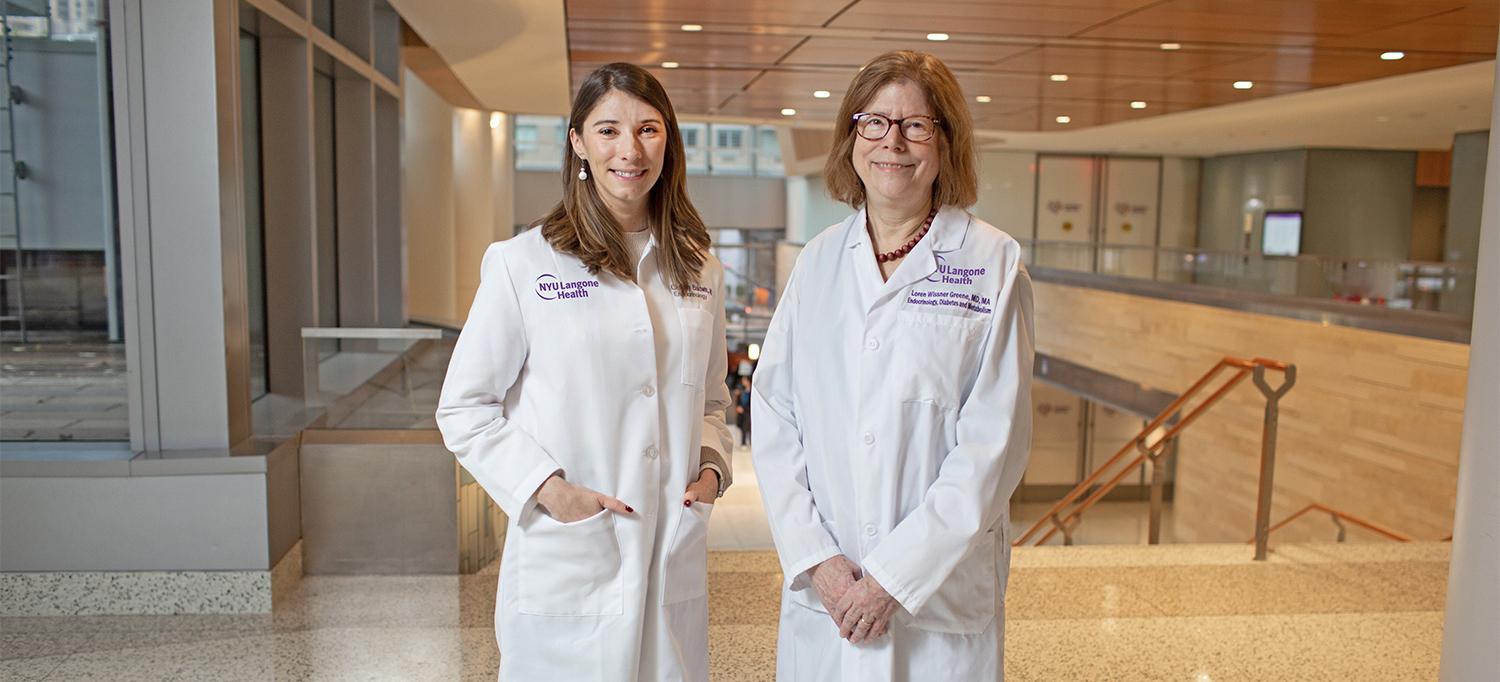
By vigilantly monitoring a patient’s calcitonin levels, endocrinologists Dr. Loren Wissner Greene and Dr. Chelsey K. Baldwin make an unusual discovery.
Photo: NYU Langone Staff
A 69-year-old woman with a multinodular thyroid came to NYU Langone Health for treatment of type 2 diabetes mellitus. Discerning a confluence of possible risk factors for thyroid cancer, her new endocrinologist took the unusual step of monitoring her calcitonin levels, which proved to be a prescient decision.
An Abundance of Caution
The patient was referred to Loren Wissner Greene, MD, clinical professor in the Department of Medicine, by her ophthalmologist, who found the woman’s diabetes was poorly controlled. In addition to metformin and insulin, she had been prescribed liraglutide by her previous endocrinologist and had been taking it for more than a year. As Dr. Greene considered the patient’s therapeutic regimen, the latter medication stood out as potentially problematic.
Liraglutide is a glucagon-like peptide receptor agonist (GLP-1 RA), a drug class of growing popularity owing to its efficacy in treating both diabetes and obesity. However, this class of medications presents significant safety concerns—including a causal, dose-dependent association with medullary thyroid cancer (MTC) in rodent models. Preclinical studies show that GLP-1 receptors on thyroid C cells mediate calcitonin production and proliferation in rats and mice, such that rising calcitonin levels are a marker for MTC in those animals.
To date, clinical trials have shown no definitive risk of MTC, a rare form of thyroid cancer, in humans treated with GLP-1 RA drugs. Indeed, healthy human C cells do not express GLP-1 receptors, and such receptors are present in only 27 percent of human MTCs. Nonetheless, the rodent studies’ association between these medications and MTC prompted the U.S. Food and Drug Administration to mandate continuing studies. A black box warning on liraglutide cautions against use of the drug by patients who have multiple endocrine neoplasia type 2 or a personal or family history of MTC.
The patient had no such history—or at least none that was known. Her prior endocrinologist had once sent her for a needle biopsy of a suspicious lesion, but it had tested as benign. Still, because of the history of such a nodule—and because multinodular goiter may be associated with a higher risk of thyroid cancer—Dr. Greene deemed it prudent to track the patient’s calcitonin level as she continued on liraglutide therapy.
She saw no reason to switch the woman to an SGLT-2 inhibitor since such drugs could pose hazards of their own. “When I first tested her, her levels were slightly elevated, but not worryingly so,” Dr. Greene recalls. “I thought it best to watch and wait.”
A Rare Discovery
Over 18 months, the woman’s diabetes control improved on liraglutide, but her calcitonin levels continued to creep upward. Concerned by this trend, Dr. Greene referred her for a thyroid ultrasound. Imaging showed a slightly larger suspicious nodule. And this time, a fine-needle biopsy identified it as medullary carcinoma.
At NYU Langone’s monthly interdisciplinary thyroid conference, the assembled clinicians—endocrinologists, surgeons, cytologists, ultrasound radiologists, and nuclear medicine specialists—discussed the best way to proceed. Some argued for a hemithyroidectomy, but Dr. Greene decided that a full excision would be safer, given that MTC (unlike other types) cannot be treated with radioactive iodine if partial surgery leaves some malignant cells behind.
“The patient led her church choir, and she was very worried that the procedure might harm her voice,” says Dr. Greene. Happily, however, the thyroidectomy left her vocal cords intact. Tissue analysis determined that the surgery also removed two previously undetected papillary tumors. The patient recovered fully and remained cancer-free at the one-year follow-up.
Dr. Greene is currently working with researchers at other institutions to identify similar incidences of MTC associated with GLP-1 RA diabetes medications in patients with multinodular goiter; so far, she and her colleagues have found another two. She presented a poster on this case at the 2019 American Thyroid Association (ATA) meeting with Chelsey K. Baldwin, MD, clinical instructor of medicine, who assisted in treatment.