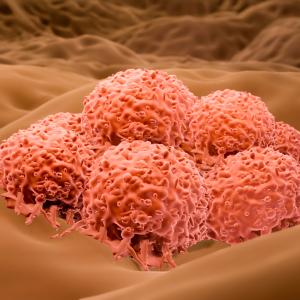
Photo: Science Photo Library/Getty
A mysterious piece of genetic material restrains the spread of skin cancer cells, but is frequently lost as they mature, a new study finds.
Published online January 13 in Cancer Cell, the new work revolves around circular RNA, a recently described type of ribonucleic acid (RNA). Typically, DNA blueprints are converted into RNA and then into proteins with cellular functions. While most RNA are linear molecules, some form circles when their ends loop around and attach. Instead of encoding proteins, circular RNA, or circRNA, seem to be part of complex regulatory systems, but their functions are still unclear, say the study authors.
Led by researchers at NYU Grossman School of Medicine, the new study in cell cultures and mice is the first to show that a circRNA called CDR1as blocks the aggressive spread of melanoma cancers, and that its loss promotes it. A study analysis of human melanoma tissues also linked higher CDR1as levels with increased survival.
In patients that die from melanoma, the most lethal form of skin cancer, the aggressive spread, or metastasis, of cancer cells is the primary cause of death. Cancer cells arise from normal cells because of genetic errors, but changes in DNA do not fully explain how the cells spread.
“Our study provides new insights into melanoma aggressive behavior, and is the first to expose a circRNA as a suppressor of metastasis,” says senior study author Eva M. Hernando, PhD, associate professor in the Department of Pathology at NYU Langone Health.
“We found CDR1as restrains a known pro-cancer protein called IGF2BP3, revealing a new function of CDR1as that may have therapeutic implications,” adds first author Douglas S. Hanniford, PhD, an instructor in the same department.
Spread Follows Loss of Restraint
Recent work had suggested previously unknown functions for circRNAs, including their binding with proteins that attach to RNA to influence cell functions. Specifically, the new study reveals that metastasis of melanomas proceeds when the interaction between CDR1as and the RNA-binding protein IGF2BP3 is disrupted.
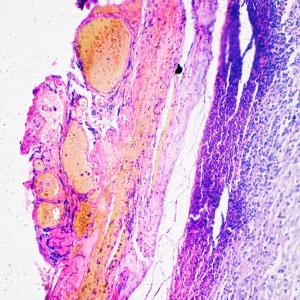
If CDR1as is active, researchers say, IGF2BP3 proteins bind to its circular RNA molecules, instead of attaching to other RNAs that code for pro-metastatic proteins. When CDR1as was removed using molecular techniques, IGF2BP3 was free to promote cancer cell invasion, which occurs when cells penetrate skin layers and spread to distant organs.
The study identifies the source of CDR1as in cells as LINC00632, an example of yet another class of RNA called long noncoding RNA. Experiments revealed further that an “epigenetic” mechanism in melanoma cells silences the LINC00632 gene, which halts CDR1as production.
Epigenetic changes adjust the operation of genes without changing their DNA itself, researchers say. These include the attachment of molecules called methyl groups to histones, the “spools” around which DNA chains are wrapped. Methylation status determines whether a given stretch of DNA is unwound and accessible; or instead compacted, with the genes residing there silenced, researchers say.
The new study found that a particular histone methylation, H3K27me3, silences the gene for LINC00632 in melanoma cells starting to spread, which come to lack CDR1as. The authors say that this interaction could represent a mechanism that helps cells migrate during normal fetal development, but that then drives cancer spread when it mistakenly re-occurs in tumors.
Along with Dr. Hernando, study authors in the Department of Pathology at NYU Langone were first author Dr. Douglas S. Hanniford; Alejandro Ulloa; Alcida Karz; Rana Moubarak, PhD; Maria Gabriela Berzoti-Coelho; Veronica Davalos; Karin C. Lilja, PhD; Jochen Imig, PhD; Andreas Kloetgen, PhD; and Iannis Aifantis, PhD. Additional NYU Langone authors were Iman Osman, MD, in the Departments of Urology and Medicine, Pamela Wu in the Institute for Systems Genetics, and Varshini Vasudevaraja of the Applied Bioinformatics Laboratories. Also authors were Beatriz Sánchez-Sendra and Carlos Monteagudo, MD, PhD, of the University of Valencia, Spain; Tommaso Tabaglio, PhD, and Ernesto Guccione, PhD, of the Icahn School of Medicine at Mount Sinai, previously at the Agency for Science, Technology, and Research in Singapore.
The study was supported by National Institutes of Health grants R01CA155234, R01CA163891, R01CA2022027, T32 CA009161-37, P30CA016087, S10OD01058 and S10OD018338; as well as by U.S. Department of Defense grant W81XWH-16-1-0437, Sào Paulo Research Foundation grant 2017/23501-6, Instituto de Salud Carlos III grants PI13/02786 and PI17/02019, FEDER European funds, and the Regional Valencian Ministry of Education PROMETEO grant II/2015/009.
Media Inquiries
Greg Williams
Phone: 212-404-3500
gregory.williams@nyulangone.org