Photo: Getty Images/John Fedele
Antenatal hydronephrosis, a finding observed in 1 percent to 2 percent of pregnancies on routine ultrasound during the second trimester, is often transient and clinically insignificant, but it also may represent a congenital anomaly of the kidney or the urinary tract that can result in impaired renal development or injury to the nephron.
The congenital anomalies of the kidney or urinary tract most commonly implicated in fetal hydronephrosis are ureteropelvic junction obstruction and vesicoureteral reflux (VUR), with other causes including urethral atresia, posterior urethral valves, megaureter, ureterocele, ectopic ureter, and multicystic dysplastic kidney.
Two patients with fetal hydronephrosis were recently referred to Ellen Shapiro, MD, professor of urology and director of pediatric urology, for evaluation and management. Collaborating with radiologists skilled in urological diagnostic imaging, the Pediatric Urology team at Hassenfeld Children’s Hospital at NYU Langone worked with the parents to provide them with individualized options and the best possible outcomes.
Renal Pelvis Dilation and Other Indicators Predictive Of Congenital Anomalies
The timing of prenatal ultrasonography is critical to detection of congenital anomalies of the kidney and the urinary tract. The fetal kidney can be visualized on ultrasound at 12 to 15 weeks’ gestation, but significant disease may be difficult to detect before differentiation of the renal cortex and the medulla, which occurs at 20 to 25 weeks’ gestation. Ultrasound allows measurement of the anterior-posterior renal pelvis diameter (RPD) and evaluation of calyceal dilation, renal parenchymal thickness and appearance, and abnormalities of the bladder or ureters. Although nephrogenesis is complete by 36 weeks’ gestation, the impact of continuing compression of the renal parenchyma on the ultimate endowment of healthy nephrons is unknown.
Anterior-posterior RPD measured in the transverse plane provides an index of hydronephrosis severity. An abnormal RPD has been defined in the National Institute of Child Health and Human Development’s 2014 Executive Summary on Fetal Imaging as 4 mm or greater in the second trimester and 7 mm or greater at 32 weeks or more, with postnatal radiographic evaluation recommended.
Mild hydronephrosis is commonly found in association with Down syndrome and should prompt evaluation of fetal anatomy to identify other congenital anomalies.4 RPD greater than 10 mm in the second trimester and/or greater than 15 mm in the third trimester are associated with increased risk of congenital anomalies of the kidney and urinary tract. Progressive antenatal dilation of the renal pelvis increases the likelihood of the need for postnatal surgical intervention. The urinary tract dilation (UTD) classification system for antenatal and postnatal hydronephrosis is based on ultrasound parameters associated with increased risk, including parenchymal changes, ureteral dilation, bilateral involvement, bladder abnormalities, and oligohydramnios.
Case 1: Progressive Postnatal Dilation Leads to Surgical Intervention and Significant Improvement
At 20 weeks’ gestation, a 35-year-old female had a routine ultrasound that identified a left anterior-posterior RPD of 8 mm with a normal right kidney and ureters. At 38 weeks’ gestation, ultrasound revealed a normal bladder and ureters and a left RPD of 2.2 cm, with peripheral calyceal dilation. mniotic fluid volume was normal. The neonate had an Apgar score of 91/95 upon delivery at 40 weeks.
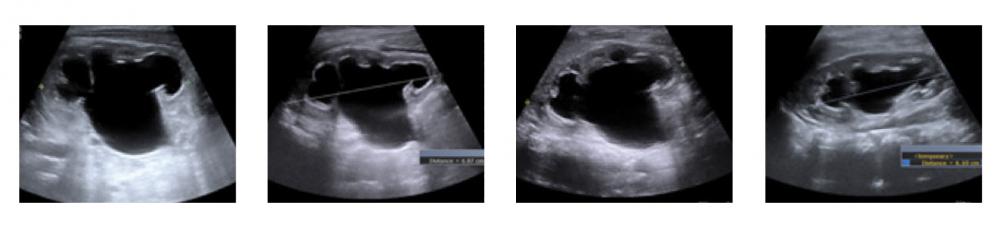
The initial postnatal ultrasound (Figure 1A) revealed a right kidney with UTD P3. There was no reflux on voiding cystourethrography (VCUG). At 6 weeks, MAG3 scan showed the right kidney contributed 60 percent of total renal function and the left kidney contributed 40 percent. Following Lasix, there was delayed drainage on the left. A second ultrasound (Figure 1B) showed no change, but the family decided to delay recommended surgery. At three months, there was a slight increase in hydronephrosis on the left (Figure 1C), and a dismembered left pyeloplasty was performed. At three months postop, ultrasound showed improvement of hydronephrosis and interval growth of the kidneys (Figure 1D).
Postnatal Management Challenges: Limit Testing and Intervention in Low-Risk Cases
Predictive factors can differentiate significant disease from mild or transient hydronephrosis and thus limit unnecessary testing. The first postnatal ultrasound is performed after 48 hours, when the neonate is volume-repleted.
Limit Intervention While Providing Close Follow-Up in High-Risk Cases
An approach based on risk stratification and monitoring reduces unnecessary testing and treatment but allows timely intervention when necessary to limit renal damage. In patients with unilateral congenital anomaly of the kidney or the urinary tract, serial ultrasound is indicated to monitor mild or moderate obstructive uropathy and to assess compensatory growth in the unaffected kidney.
Evaluation of fetal hydronephrosis includes a dynamic renal scan (MAG3), to differentiate obstructive from nonobstructive causes of hydronephrosis. VCUG is the definitive study to identify VUR and to assess the lower urinary tract. If the results of VCUG will affect case management, it may be indicated for all infants with significant hydronephrosis, ureteral dilation, thick-walled bladder, or urethral pathology and for male infants who are likely to have urethral pathology. Infants at high risk for VUR should also be treated with prophylactic antibiotics.
Case 2: Surgery Delayed after Improvement, with Subsequent Resolution of Hydronephrosis
A 31-year-old female had a normal 20-week structural ultrasound. At 32 weeks, ultrasound showed a right RPD of 1.5 cm with peripheral calyceal dilation (UTD A2–3). The left kidney, ureters, and bladder appeared normal. At 37 weeks, the anterior-posterior RPD was 2.0 cm (UTD A2–3). The amniotic fluid volume was normal. Vaginal delivery at 40 weeks was uneventful, with the neonate having an Apgar score of 91/95.
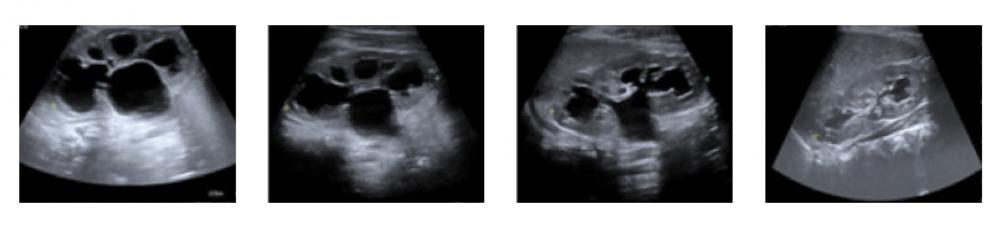
The first postnatal sonogram (Figure 2A) at 1 week of age showed the right kidney with UTD P3. A VCUG showed no reflux. The MAG3 scan at 6 weeks of age demonstrated contribution to total renal function of 35 percent from the right kidney and 65 percent from the left. Following Lasix, poor drainage on the right was noted. A second renal sonogram (Figure 2B) showed a slight improvement of hydronephrosis, so surgery was not recommended. Renal sonogram at 3 months (Figure 2C) showed definite improvement in the degree of right hydronephrosis. At 1 year, renal ultrasound showed almost complete resolution of hydronephrosis, with decompression of the collecting system (Figure 2D).
Timing of Intervention: A Delicate Balance
It is unclear whether compression of the renal pyramids and renal parenchyma affects ultimate healthy nephron endowment or whether function in an obstructed kidney can be completely recovered, but early intervention by a skilled pediatric urologist has been demonstrated to be effective in restoring compromised renal function. When managing fetal hydronephrosis, any delay in intervention should be accompanied by close follow-up, with timely surgical correction before irreparable damage occurs.
References
- Hamilton BE, Martin JA, Ventura SJ. Births: preliminary data for 2012. Natl Vital Stat Rep. 2013;62(3):1-20.
- Nguyen HT, Benson CB, Bromley B, Campbell JB, Chow J, Coleman B, Cooper C, Crino J, Darge K, Herndon CD, Odibo AO, Somers MJ, Stein DR. Multidisciplinary consensus on the classification of prenatal and postnatal urinary tract dilation (UTD classification system). J Pediatr Urol. 2014;10(6):982-998.
- Signorelli M, Cerri V, Taddei F, Groli C, Bianchi UA. Prenatal diagnosis and management of mild fetal pyelectasis: implications for neonatal outcome and follow-up. Eur J Obstet Gynecol Reprod Biol. 2005;118(2):154-159.
- Bromley B, Lieberman E, Shipp TD, Benacerraf BR. The genetic sonogram: a method of risk assessment for Down syndrome in the second trimester. J Ultrasound Med. 2002;21(10): 1087-109.