The multidisciplinary team of physicians at the Head and Neck Center, including Dr. Michael J. Persky, utilize minimally invasive and robotic surgical techniques as well as advanced reconstruction methods to improve patient outcomes.
Photo: NYU Langone Staff
With the goal of improving patient outcomes using less invasive, more efficacious approaches, a multidisciplinary team of physicians at NYU Langone’s Head and Neck Center continues to pioneer leading-edge minimally invasive and robotic surgical techniques alongside advanced reconstruction methods. Combining focused expertise in the specialty with a dedicated unit equipped with advanced technologies, the team is pushing the boundaries of surgical treatment with greater precision and individualized options for patients with a range of head and neck conditions.
Enhancing Patient Selection for Robotic Surgery
With optimal application, robotic approaches offer several advantages, including more precise surgical targeting and decreased morbidity. The team’s deep surgical expertise is critically important to match NYU Langone’s available technology—which includes the single-port robot, the most advanced robot available for head and neck surgery—with the patients who will accrue the greatest benefit.
“We maintain careful, patient-centric criteria to determine when the robot is indicated, rather than deferring to its use simply because it’s there,” notes Michael J. Persky, MD, assistant professor in the Department of Otolaryngology—Head and Neck Surgery and director of head and neck robotic surgery.
Patient evaluation involves a high degree of collaboration among a multidisciplinary team uniquely experienced in, and dedicated to, coordinated head and neck care. “It’s highly unusual for patients to consult with their surgeons, medical oncologists, and radiation oncologists—all specialty trained in the head and neck—from a single point of care,” notes Mark S. Persky, MD, professor in the Department of Otolaryngology—Head and Neck Surgery. “The centralized expertise is critical to inform the most efficacious plan to treat each individual patient—including the decision of whether to utilize a robot in surgery.”
Together, the team considers several variables when evaluating the surgical approach and potential robot application, including the stage of the head or neck tumor, the likelihood of achieving negative margins, and lymph node metastasis. For patients amenable to the robotic approach, positive outcomes include complete tumor resection with a less invasive surgery and a reduced need for adjuvant therapy without recurrent tumor. Often, chemotherapy can be bypassed completely. “These patients do much better in the long term, with speech and swallowing intact and without the compounding morbidity of high-dose radiation treatment,” Dr. Michael Persky adds. “But it can backfire if the robot is used without discretion on patients with adverse pathology, inadvertently leading to unnecessarily intensified treatment that could have been avoided.”
Physicians at the Head and Neck Center are also applying a robotic approach for patients with unknown primary tumors in the back of the throat, who previously required widespread radiation treatment of the potential primary sites. This enables targeted tissue removal in the suspected area with a high degree of accuracy. “We used to take biopsies hoping to determine the tumor site—but their elusive location often made that approach difficult,” notes Dr. Michael Persky. “Now we’re positively identifying the primary tumor site and achieving negative margins more often than not, enabling directed and site-specific radiation rather than radiating the entire oropharynx.”
Complex Malformations Addressed with Collaboration and Experience
Careful, multidisciplinary surgical planning and expertise gained through surgical experience enable the head and neck team to treat conditions few physicians are willing or able to address. In collaboration with interventional radiologists at the center, Dr. Mark Persky is developing a highly specialized multidisciplinary surgical group with expertise in treating patients with complex vascular malformations and vascular head and neck tumors.
Such high-flow malformations can be quite extensive and carry significant risk of life-threatening complications during treatment, such as bleeding and irreversible damage to involved organs, depending on their size and location. Dr. Mark Persky is among few physicians who have vast experience and expertise in treating these malformations with a combination of surgery and embolization. With the growing vascular malformation group, Dr. Mark Persky will build on a history of surgical innovation at the center, where the team has applied new techniques to safely deliver positive outcomes for patients. Additional advances in this field have also resulted in treating select patients with vascular malformation with sclerosing therapy or medical therapy.
Surgical success depends squarely on the shared experience and combined expertise of the surgeon and the interventional radiologist. Over time, that synthesis at the center has helped the team to perform the procedures more quickly, with reductions in blood loss and other complications. Center specialists use regular tumor board–style discussions to learn from each case and strengthen their multidisciplinary approach, and they routinely operate with younger faculty to help them further their own experience in these cases.
“These surgeries are incredibly complex, and no innovation can supersede the instincts that develop over time by performing them again and again,” says Dr. Mark Persky. “You need to be cognizant during surgery to understand and appreciate what is happening and, if necessary, modify the procedure to obtain the ideal result.”
Reaching Greater Nuance in Reconstruction
As primary surgeries become safer and more efficient, experts at the center are working across disciplines to enhance reconstructive techniques, approaching highly complex cases with a combination of nuanced surgical practices and advanced medical modeling. Virtual surgical planning has become an important part of shaping both the extirpation and the reconstruction portions of these surgeries. The approach fosters more thoughtful and seamless planning between the extirpative and reconstructive teams, creating more sophisticated reconstructions that lead to better outcomes.
For patients with tumors of the mouth or jaw, advances in three-dimensional (3D) holographic technology support greater precision in preoperative planning, enabling both a mandibular replacement and functional dental restoration in the same surgery. In contrast, less nuanced surgical methods may limit cosmetic appearance and function if they do not mirror the jaw’s natural angles, and they often require multiple surgeries to complete the reconstruction and dental rehabilitation. Surgeons use medical models to plan the surgeries along with patient-specific 3D print hardware, allowing the exact placement of the rigid fixation hardware and the osseointegrated implants in one surgery.
“These are extremely sophisticated reconstructions in highly complex patients whom other centers may hesitate to operate on at all,” notes Adam S. Jacobson, MD, associate professor in the Department of Otolaryngology—Head and Neck Surgery and director of the Division of Head and Neck Surgery. “Our ability to mimic a patient’s natural anatomy makes every difference in their outcome, both cosmetically and functionally.”
The center is also expanding free flap approaches from an array of donor sites to provide optimal tissue for each patient. With Jamie P. Levine, MD, associate professor in the Hansjörg Wyss Department of Plastic Surgery, Dr. Jacobson has pioneered the medial sural artery perforator flap—taken from the back of the calf and constituted of skin, soft tissue, and some underlying fascia—in head and neck reconstruction. “That particular flap was first described years ago for lower extremity reconstruction,” notes Dr. Jacobson. “The idea to use it in the head and neck came from our team’s ongoing push to think broadly about possibilities for better patient outcomes.”
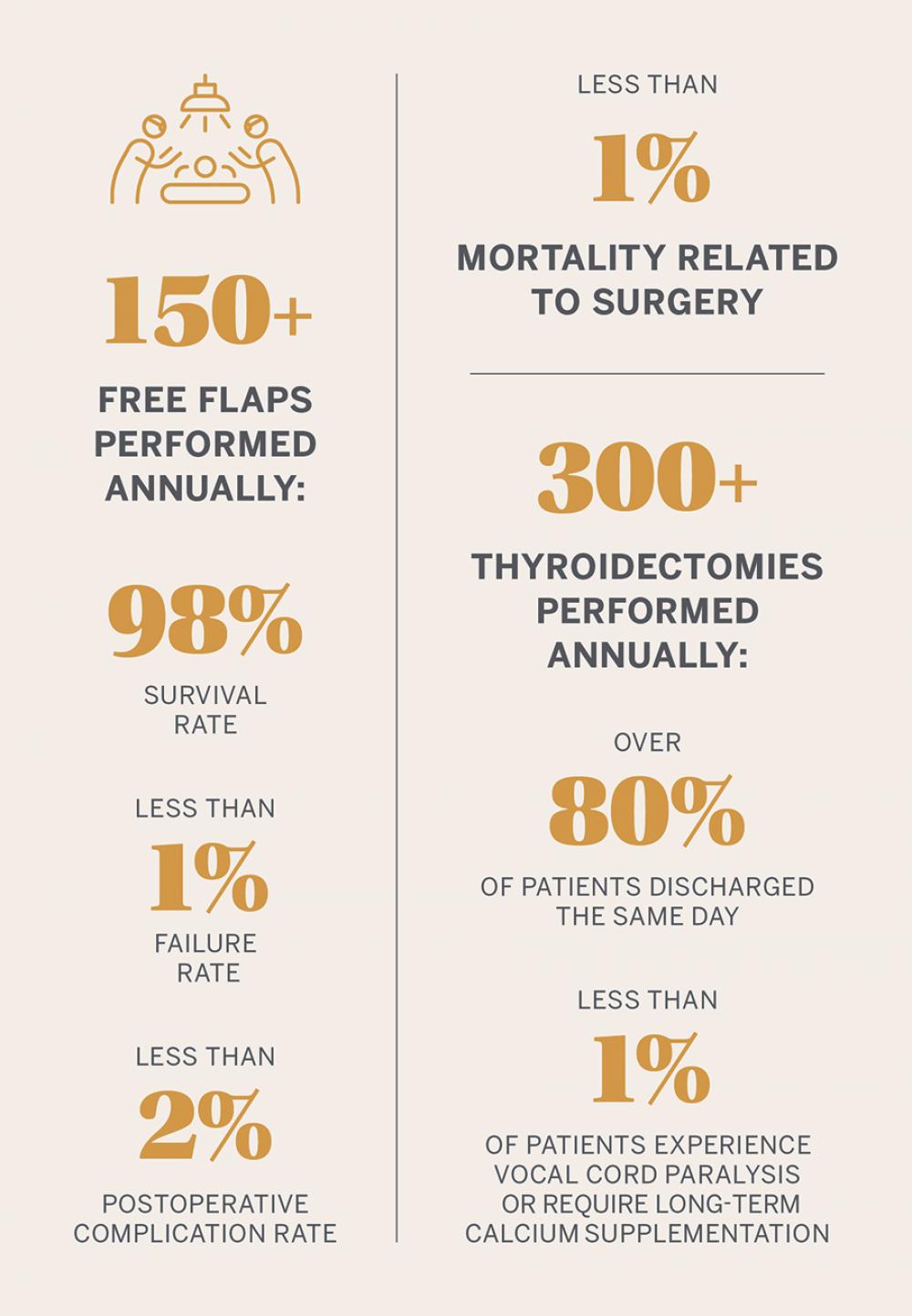
Dr. Jacobson and his team perform more than 150 free flap approaches each year, utilizing 3D planning to carefully model each surgery for the best possible outcomes. When possible, they are also extending the techniques to correct earlier reconstructions in certain patients. “The goal is to restore patients to their pre-disease state,” he notes. “With technology advancing, we can perform more thoughtful reconstructions and more closely approach that state than ever before.”
A Shared Emphasis on Innovation
These novel surgical methods, treatment approaches, and reconstruction techniques all demand a high degree of multidisciplinary collaboration among head and neck surgeons, radiologists, pathologists, basic science researchers, nurses, maxillofacial prosthodontists, and other specialists aligned to deliver forward-thinking care that evolves with new understanding. “I try to learn one thing from every case, especially the most complex cases,” notes Dr. Mark Persky. “Imagine how many lessons I’ve incorporated into future patient care over the thousands of cases I’ve treated.”