Key Finding of Dueling Bacterial Toxins Shows Why Hospital Superbug is so Deadly & its Close Relatives Are Not
New research led by NYU Langone has uncovered why a particular strain of Staphylococcus aureus—known as HA-MRSA—becomes more deadly than other variations. These new findings open up possible new pathways to vaccine development against this bacterium, which the Centers for Disease Control and Prevention says accounts for over 10,000 deaths annually, mostly among hospital patients.
In a series of experiments in mice and in human immune cells in the lab, recently published in the journal Nature Communications online September 2, the NYU Langone team found that the presence or absence of dueling toxins, or bacterial poisons, appears to explain the major difference between HA-MRSA, and its less virulent and more common, community-based cousin, CA-MRSA, the two main types of MRSA infection.
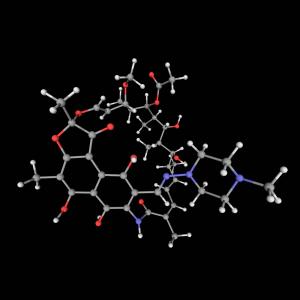
Specifically, the researchers say, a key toxin, called LUK-PV, secreted only by community-acquired MRSA, counteracts the effects of another more deadly toxin, LUK-ED, secreted by both forms of the bacterium.
Researchers say both LUK-PV and LUK-ED are leukotoxins that target and poison immune system white blood cells meant to fight the bacterial infection, but LUK-PV is only secreted by community-acquired MRSA, or methicillin-resistant S. aureus.
According to study senior investigator and NYU Langone microbiologist Victor Torres, PhD, the newly discovered competing or “antagonistic” relationship between the two bacterial toxins helps explain how community-acquired MRSA is far more widespread and less deadly than hospital-acquired MRSA.
“Essentially, in community-acquired MRSA, the toxins neutralize each other, while in the hospital superbug form, they do not,” says Torres.
Torres also says that these study results challenge the current mindset for finding a vaccine against staphylococcal infections, including MRSA.
“No longer can we take an isolated approach of trying to target and block one leukotoxin at a time,” says Torres, an associate professor at NYU Langone. “We have to take a broader view of the pathogen and will likely have to target more than one toxin in order to develop an effective vaccine.”
In a separate set of laboratory experiments previously described in the journal Cell Host & Microbe online August 27, researchers at Torres’ laboratory and colleagues in the Netherlands, France, and Australia showed how LUK-ED attacked red blood cells to obtain nutrients, most notably iron, essential for its rapid growth and infection. The international team found that the toxin split apart the red blood cells by attaching itself first to their so-called Duffy antigen protein receptor, the same receptor widely known to be targeted by the human Plasmodium malarial parasites.
Torres says his research is making clearer that multiple bacterial toxins, such as the five known to be contained in community-acquired MRSA, react very differently on their own than when combined—because they can counteract each other.
His team next plans to analyze the biological mechanisms by which LUK-PV and LUK-ED target, attach and destroy white and red blood cells, making their host more vulnerable to infection. Other experiments are set to determine how widespread bacteremia from staphylococcal infections actually shuts down the mammalian body, causing death.
Torres also has plans to study groups of Africans known to be genetically deficient in Duffy antigens and, hence, more resistant to malaria, to see if they are resistant to staphylococcal infection, as well.
Funding support for both studies, which took four years to complete, was provided by the National Institute of Allergy and Infectious Diseases, a member of the National Institutes of Health. Corresponding grant numbers are R01 AI099394 and R01 AI105129. Additional study funding support was provided by the Burroughs Wellcome Fund.
Under a licensing agreement between New York University and Janssen Biotech Inc., of Horsham, Pa. (a subsidiary of pharmaceutical manufacturer Johnson and Johnson, of New Brunswick, NJ), Torres is entitled to a share of commercialization revenue received by the University on the development and sales of products tied to development of a staphylococcal vaccine or toxin inhibitors, in addition to research funds. The terms of these arrangements are being managed by NYU in accordance with its conflict of interest policies.
Besides Torres, other NYU Langone scientists involved in this research were Pauline Yoong, PhD; Tamara Reyes-Robles, PhD; and Kristina Boguslawski, PhD. Additional research support was provided by Andras Spaan, PhD; Cedric Badiou, PhD; Francois Vandenesch, PhD; and Thomas Henry, PhD, at the Centre de Recherche en Infectiologie, in Lyon, France; and Carla de Haas, PhD; Kok van Kessel, PhD; and Jos van Strijp, PhD, at the University Medical Center in Utrecht, the Netherlands; and Sylvie Cochet, PhD; Caroline Le Van Kim, PhD; Yves Colin, PhD, at the Institut National de la Sante et de la Recherche Medicale, in Paris; and Christopher Day, PhD; and Michael Jennings, PhD, at Griffith University in Gold Coast, Australia.
Media Inquiries
David March
Phone: 212-404-3528
david.march@nyumc.org